Pustules: causes, symptoms, diagnosis, and treatment
About the symptom
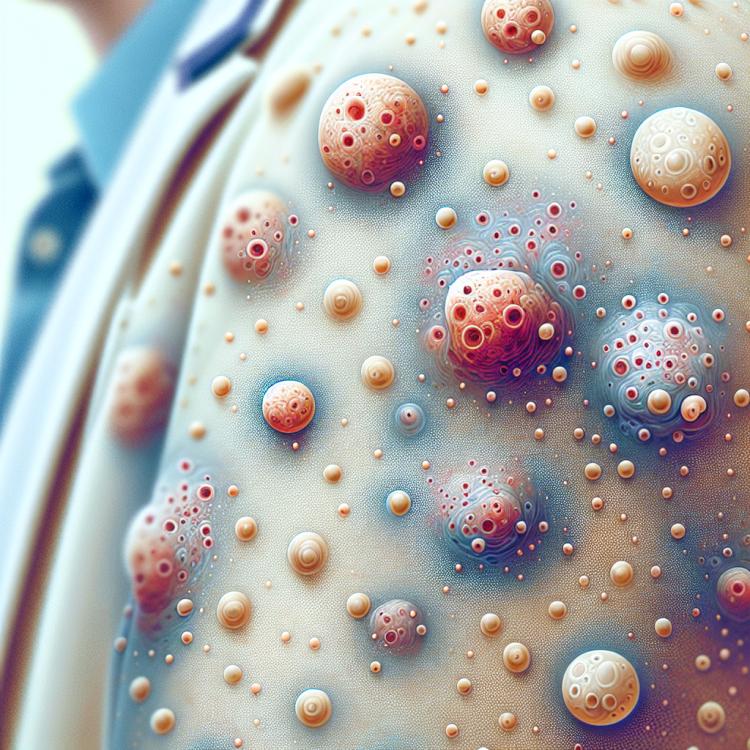
Pustules are small blisters on the skin filled with pus, which can occur in various parts of the body. They can vary in size and shape, and are often accompanied by redness and swelling of the surrounding skin. The main symptom of pustules is itching, which can cause discomfort and concern for patients. In some cases, pustules may rupture on their own, leading to the discharge of pus and possible improvement in condition; however, in most cases, medical intervention is required for quicker recovery.
There are also additional symptoms that may accompany the appearance of pustules. These include fever, general malaise, and tenderness in the area of inflammation. It is especially important to pay attention to the state of the immune system, as a weakened body may be more prone to the occurrence of pustules. It is important to remember that the appearance of pustules can be caused by various factors, such as infectious diseases, failure to adhere to hygiene standards, as well as allergic reactions, so when such symptoms occur, it is recommended to see a doctor for accurate diagnosis and appropriate treatment.
Diseases
Pustules are a sign of various diseases associated with infections that can affect the skin as well as the mucous membranes of the body. They can occur as a result of bacteria, fungi, or viruses, leading to the appearance of pustules or purulent formations on the skin. It is important to note that the presence of pustules is not an independent disease but a symptom that may indicate more serious health issues.
Since pustules can arise due to various infections, it is important to consult a doctor for diagnosis and to determine the exact cause of their appearance. The main conditions that provoke the development of pustules include a weakened immune system, the presence of chronic diseases, improper skin care, and non-compliance with hygiene rules.
- Pustular psoriasis
- Streptococcal infection
- Staphylococcal infection
- Furuncles
- Impetigo
- Cutaneous candidiasis
- Acne (pimple rash)
- Purulent bedsores
Diagnosis
The diagnosis of pustules begins with a thorough medical examination and analysis of the clinical picture. The doctor assesses the existing symptoms, such as the size, color, and localization of the pustules, as well as accompanying manifestations like itching, swelling, or pain. It is important to consider the patient’s history: the presence of allergies, previous skin conditions, or systemic infections. This allows for a complete understanding of the patient’s health status and helps identify potential causes for the appearance of pustules.
For a more accurate diagnosis, additional investigations may be ordered. These include tests for infection, skin scrapings for microscopy, as well as bacteriological cultures. These diagnostic procedures help identify the causes of pustules and determine the sensitivity of the identified microorganisms to antibiotics, which is key to effective treatment.
- Complete blood count
- Bacteriological culture on nutrient media
- Skin scraping for microscopic examination
- Allergy tests
- Serological tests for infectious diseases
Which doctor to consult
When pustules appear on the skin, it is important not to ignore this condition and seek medical help. Initially, it is advisable to visit a dermatologist — a specialist who diagnoses and treats skin diseases. They will help determine the nature of the pustules and provide recommendations for appropriate treatment. Temporarily, the dermatologist may prescribe anti-inflammatory agents or antibiotics if necessary.
If the pustules are caused by internal diseases or infections, the dermatologist may need to consult other specialists. For example, a therapist or infectious disease specialist can assess the overall health of the body and identify possible systemic diseases that may contribute to such symptoms. It is important to remember that the lack of adequate treatment can lead to the spread of infection and even other complications.
- Dermatologist
- Therapist
- Infectious disease specialist
- Endocrinologist (in case of suspected hormonal disorders)
- Allergist (if an allergic reaction is suspected)
Types of Pustules
Pustules can manifest in various forms and types, depending on the reasons for their appearance and localization. The most common types of pustules include furuncles, carbuncles, pustules, and abscesses. Furuncles are deep inflammatory processes that occur in hair follicles, usually accompanied by redness, swelling, and the formation of purulent content. Carbuncles consist of several interconnected furuncles and can cause more serious manifestations, such as fatigue, fever, and painful sensations.
Pustules are small pustules that most often occur in skin diseases such as acne or streptoderma. They can have a round, spherical shape and can be localized on the face, neck, or other areas of the body. Abscesses are collections of pus within the tissue and often require surgical intervention for removal. Each of these types of pustules requires an individual approach to treatment, as they may indicate various diseases and health conditions.
- Furuncles
- Carbuncles
- Pustules
- Abscesses
- Purulent skin inflammations
Causes of Pustules
Pustules are the result of an inflammatory process that occurs in the deeper layers of the skin. They can appear for various reasons, including bacterial infections, viral diseases, and allergic reactions. The most common cause of pustules is an infection caused by staphylococci or streptococci that penetrate the skin through cuts, cracks, or other injuries.
Additionally, the occurrence of pustules may be related to factors such as immune system diseases, which lead to a decrease in the body’s defensive functions. Pustules also often occur in patients with chronic diseases, such as diabetes, which impairs tissue healing. External factors such as increased humidity, heat, and a lack of personal hygiene can also contribute to the formation of pustules.
- Bacterial infections
- Viral infections
- Allergic reactions
- Skin diseases (e.g., eczema, psoriasis)
- Chronic diseases (e.g., diabetes)
- Poor hygiene practices
Common Related Pathologies
Pustules on the skin can be not only an independent disease but also a symptom of various pathologies associated with weakened immune system or the presence of infectious processes in the body. One of the most common pathologies is pyoderma, characterized by the appearance of multiple pustules on the skin. This infection can be triggered by various microorganisms, including staphylococci and streptococci, especially if there are injuries on the skin, such as cuts or abrasions.
Another related pathology is impetigo, a highly contagious skin disease that occurs as a result of infection by streptococci or staphylococci. Impetigo often manifests as blisters and crusts, making it similar to pustular diseases. It’s also worth mentioning furuncles and carbuncles, which represent deeper infections of hair follicles, leading to the formation of large pustules accompanied by inflammation and pain.
- Pyoderma
- Impetigo
- Furunculosis
- Carbuncle
- Fungal skin infections
Expert Opinion
Pustules, or purulent formations on the skin, can be a symptom of various diseases and require careful attention. Many factors can contribute to their occurrence, including bacterial infections, allergic reactions, and vitamin deficiencies. It is important to remember that self-medication in this case can lead to complications, so consulting a specialist is essential.
Experts note that to effectively treat pustules, it is necessary to determine the cause of their occurrence. This may require additional examinations and diagnostics. The use of topical antiseptics and anti-inflammatory agents is often the first step in therapy, but the final decision regarding treatment should be made by a doctor based on the individual characteristics of the patient and the nature of the disease.
Regular visits to dermatologists and immunologists can help prevent recurrences and improve the overall condition of the skin. By discussing their condition with specialists, patients can receive valuable recommendations on skin care and lifestyle, which helps reduce the risk of pustules appearing in the future.

Treatment of Pustules
The treatment of pustules depends on their underlying cause and the severity of the inflammatory process. The primary goal of therapy is to eliminate the infectious agent, reduce inflammation, and prevent the spread of the disease. The doctor may prescribe anti-inflammatory medications, antibacterial and antifungal agents, as well as immunomodulators to improve the overall level of immune protection in the body.
In addition to medication therapy, it is important to follow personal hygiene rules and monitor the condition of the skin. In the presence of purulent formations, it is not recommended to open or squeeze them on your own, to avoid the spread of infection and the appearance of serious complications. In some cases, surgical intervention may be required to remove purulent content or affected tissue.
- Conservative treatment using ointments and creams;
- Antibiotic therapy;
- Surgical procedures to remove pus;
- Physical therapy to accelerate healing;
- Immunomodulating agents.
Complications
Pustules, although they often seem like insignificant manifestations, can be a signal of more serious illnesses and lead to various complications if not properly treated. The most common consequences include the development of abscesses, cellulitis, and systemic infections that can affect not only the skin but also internal organs. The appearance of pustules on the skin can lead to inflammation, infections, and even sepsis in the most severe cases if the infection enters the bloodstream.
Furthermore, neglected pustules can leave behind scars and spots on the skin, negatively impacting appearance. Areas with intense sweating, such as the armpits, groin, and the area around the genitals, are especially susceptible to this. Therefore, it is important not only to monitor the symptoms but also to seek medical help promptly if any pustules arise.
- Abscess – a localized collection of pus in tissues;
- Cellulitis – diffuse purulent inflammation of subcutaneous fatty tissue;
- Sepsis – a systemic inflammatory reaction to infection;
- Scars and hyperpigmentation of the skin;
- Exacerbation of chronic skin diseases.