Oral candidiasis: symptoms, treatment, and prevention
About the Symptom
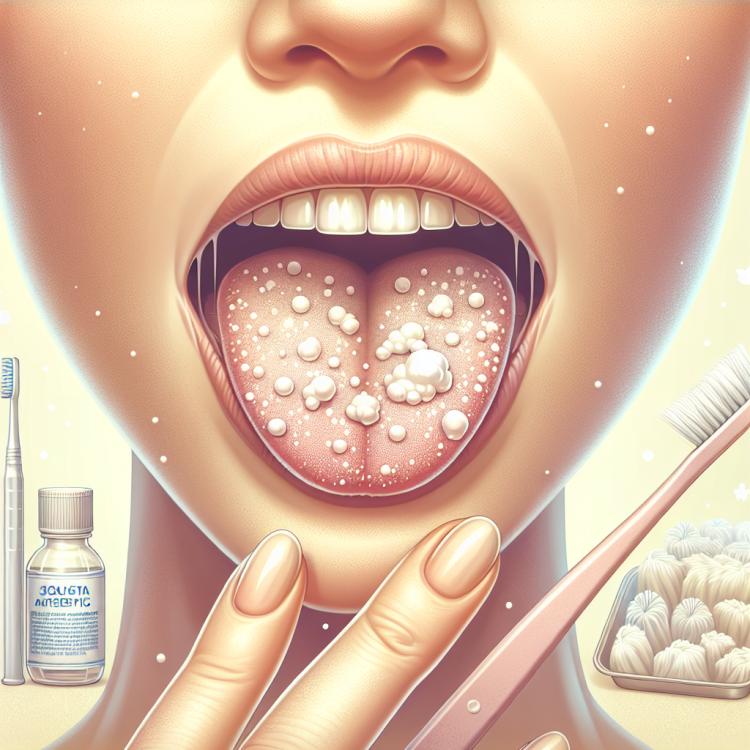
Oral candidiasis, also known as thrush, is a common fungal infection caused by the overgrowth of fungi of the genus Candida, particularly Candida albicans. The most characteristic symptoms of candidiasis include white patches on the tongue, the inner surfaces of the cheeks, gums, and palate. These patches can range from mild to extensive and are often accompanied by discomfort, including painful sores, making it difficult to eat and swallow. Patients often report a burning sensation, dryness, and discomfort, which leads to a reduced quality of life.
In addition, candidiasis may present not only with the presence of patches but also with itching in the oral area and pain that worsens when consuming acidic or spicy foods. It is important to remember that oral candidiasis can be a sign of a weakened immune system, as well as the presence of other diseases such as diabetes. Therefore, at the first signs of this condition, it is necessary to consult a doctor for proper diagnosis and effective treatment options.
Diseases
Oral thrush, also known as candidiasis of the oral cavity, is a fungal infection caused by the excessive multiplication of the fungus Candida, particularly Candida albicans. This condition often occurs in individuals with weakened immune systems, such as the elderly, newborns, and patients with chronic diseases. The main factors contributing to the development of candidiasis include prolonged use of antibiotics, corticosteroids, and chronic conditions such as diabetes or HIV infection.
Signs and symptoms of oral candidiasis may include white or yellowish patches on the tongue and inner surfaces of the cheeks, painful cracks in the corners of the mouth, as well as a burning sensation or discomfort when consuming food and beverages. Some patients may develop individual sores that can cause significant discomfort. Ignoring these symptoms can lead to complications and inflammatory processes, so timely diagnosis and treatment are crucial.
- Dry mouth;
- Difficulty swallowing;
- Painful sensations in the oral cavity;
- Bad breath;
- Difficulties wearing dentures;
- Frequent relapses of oral candidiasis;
- Difficulty perceiving taste.
Diagnosis
The diagnosis of oral candidiasis plays a key role in determining the exact diagnosis and prescribing effective treatment. Special attention is paid to clinical manifestations such as whitish plaques on the tongue and the mucous membrane of the cheeks, which are easily removed. The dentist or an infectious disease specialist conducts an examination while also inquiring about the patient’s concomitant diseases, such as diabetes or immunodeficiency, which may contribute to the development of a fungal infection.
To confirm the diagnosis, a microbiological examination may be required. This includes taking samples of saliva or tissue from the affected mucous membrane for further research. Such tests help identify not only the presence of Candida fungus but also its species affiliation, which may be important for choosing the correct therapy. In addition, other possible diagnostic procedures aimed at excluding concomitant diseases are also considered.
- Clinical examination of the oral cavity
- Microbiological study (swab, scraping)
- Saliva analysis for the presence of Candida
- Complete blood count and glucose level
- Enzyme-linked immunosorbent assay to assess the state of the immune system
Which doctor to consult
If a candidiasis of the oral cavity is suspected, it is important to consult a qualified specialist to obtain an accurate diagnosis and to prescribe adequate treatment. Usually, the first step is to visit a dentist, who will assess the condition of the oral cavity and conduct the necessary examinations. The dentist may perform basic tests and, if necessary, refer the patient to other specialists, such as an infectious disease doctor or an otolaryngologist, for a more in-depth study of the problem.
If oral candidiasis is accompanied by other symptoms, such as fever or general malaise, it is also advisable to consider consulting a therapist. This doctor will help assess the overall health condition and identify possible causes of the development of candidiasis, which can be useful for selecting the most effective treatment.
- Dentist
- Infectious disease doctor
- Otolaryngologist
- Therapist
- Immunologist
Types of Oral Candidiasis
Oral candidiasis, also known as oral thrush, is a fungal infection caused by the overgrowth of yeast fungi of the genus Candida, most commonly Candida albicans. There are several types of oral candidiasis that can present various symptoms and degrees of severity. The main types include acute candidiasis, chronic candidiasis, and candidiasis in newborns. Each of these forms requires special attention and appropriate treatment to avoid complications and recurrences of the disease.
Acute oral candidiasis usually manifests as a pronounced white coating on the mucous membrane of the mouth, which can cause painful sensations and difficulties when swallowing. Chronic candidiasis may be less noticeable, but nonetheless can cause unpleasant symptoms such as itching and discomfort. Candidiasis in newborns often occurs in the first months of life and requires a special approach to treatment, as breast milk may contain antibodies that help fight the infection. It is important to remember to seek medical advice at the first signs of symptoms.
- Acute candidiasis
- Chronic candidiasis
- Candidiasis in newborns
- Candidiasis resulting from antibiotic therapy
- Candidiasis in immunocompromised patients
Causes of Oral Candidiasis
Oral candidiasis, also known as thrush, is caused by fungi of the genus Candida, mainly Candida albicans. These microorganisms are part of the normal human microflora and usually do not cause problems. However, under certain conditions, such as a weakened immune system or disruption of the microflora balance, they can start to multiply, leading to the development of the disease. Various factors can contribute to this process, including antibiotic therapy, chronic illnesses, and dietary changes.
One of the most common causes of oral candidiasis is the use of antibiotics, which can destroy beneficial bacteria that help maintain the balance of microflora. Additionally, patients with diabetes, especially those with poorly controlled blood sugar levels, are at increased risk of developing candidiasis. Poor oral hygiene and the use of removable dentures are also significant factors, as they can create ideal conditions for fungal growth.
- Antibiotic therapy
- Diabetes
- Immunosuppression (e.g., HIV/AIDS)
- Long-term use of corticosteroids or immunomodulators
- Poor oral hygiene
- Use of dentures
Common Related Pathologies
Oral candidiasis may be associated with a number of other diseases or conditions that contribute to its development or exacerbation. One of the main causes is a reduced immune response, which can be observed in various diseases such as HIV/AIDS, diabetes, or cancer. These diseases weaken the body’s protective mechanisms, allowing fungi, including Candida, to multiply uncontrollably.
In addition, prolonged use of antibiotics or corticosteroids can lead to an imbalance of the body’s microflora, creating ideal conditions for the development of candidiasis. Conditions such as dry mouth (xerostomia) also increase the risk, as saliva plays an important role in maintaining normal oral microflora and suppressing the growth of pathogenic microorganisms.
- Diabetes
- HIV/AIDS
- Immunodeficiency states
- Systemic diseases (for example, cancer)
- Long-term antibiotic therapy
- Xerostomia (dry mouth)
Expert Opinion
Candidiasis of the oral cavity, also known as oral thrush, is an infectious disease caused by the fungus of the genus Candida, most often Candida albicans. This type of fungus normally resides in our body, but under certain circumstances, such as a weakened immune system or an imbalance in microflora, it can cause painful inflammations and discomfort. According to experts, maintaining oral health plays an important role in the prevention of candidiasis. Regular dental visits and attentive hygiene can significantly reduce the risk of developing this disease.
Treatment of oral candidiasis requires a comprehensive approach and may include both topical antifungal medications and systemic therapy, depending on the severity of the patient’s condition. Well-known medications, such as fluconazole, are widely used in various clinics and have high efficacy. Doctors also emphasize the importance of correcting underlying factors, such as diabetes and antibiotic use, which may contribute to the development of candidiasis. Timely diagnosis and professional assistance from a specialist are key to successful recovery.

Treatment of Oral Candidiasis
Treatment of oral candidiasis often requires a comprehensive approach, including both medication therapy and lifestyle changes. The main goal of treatment is to eliminate the fungal infection and restore the normal microflora of the oral cavity. It is important to note that the treatment should be conducted under the supervision of a doctor to avoid complications and relapses.
Medication for candidiasis typically includes antifungal agents that may be prescribed in the form of tablets or mouthwash solutions. Additionally, doctors may recommend probiotics to restore beneficial microflora. However, significant attention should also be given to preventive measures, such as maintaining hygiene standards and correcting nutrition.
- Antifungal medications (e.g., fluconazole, ketoconazole)
- Antiseptics for mouth rinsing
- Probiotics to restore microflora
- Diet correction (reducing sugar, moderate carbohydrate intake)
- Selecting the right hygiene products (e.g., alcohol-free toothpaste)
Complications
Oral candidiasis, if left untreated, can lead to a number of serious complications that negatively affect the overall health of the patient. One of the most common consequences is the deterioration of the body’s overall immune status. Chronic candidiasis can become a predisposing factor for the occurrence of systemic infections that can affect various organs and systems. For example, individuals with weakened immune systems, such as those undergoing chemotherapy or viral infections, are several times more at risk of the fungal infection spreading.
Additionally, candidiasis can lead to more serious illnesses, such as candidal esophagitis, which is inflammation of the esophagus and can cause pain when swallowing, as well as difficulties in eating. In rare cases, candidiasis can also cause what is known as disseminated candidiasis, which is a systemic infection capable of affecting vital organs such as the lungs or kidneys, significantly increasing the risk of serious complications like sepsis.
- Deterioration of immune status
- Candidal esophagitis
- Disseminated candidiasis
- Inflammation of other organs
- Systemic infections
FAQ
What are the main symptoms of oral candidiasis and how can it be prevented?
What are the most effective treatment methods for oral thrush?
Treatment methods for oral candidiasis may include the use of antifungal medications, such as nystatin or fluconazole, which may be prescribed in the form of suspensions or tablets, depending on the severity of the disease. It is also important to conduct various activities aimed at improving oral hygiene, which may include rinsing with antiseptic solutions. An individual approach to each patient and timely diagnosis will help achieve the best results in treatment.