Catatonic syndrome: symptoms, causes, and treatment
About the Symptom
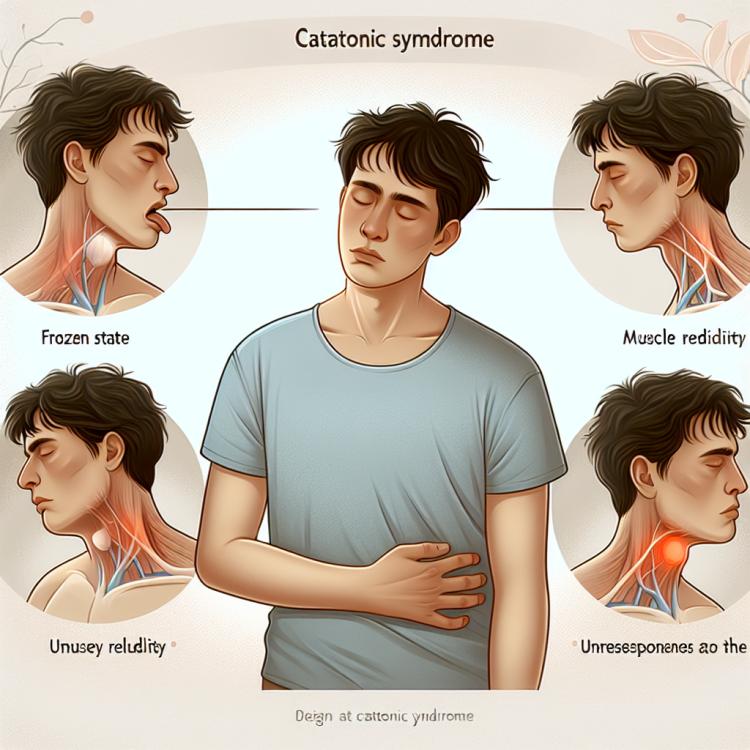
Catatonic syndrome is a psychomotor disorder characterized by the presence of pronounced disturbances in motor activity and behavior. The main symptoms of catatonia may include hyperkinesis, which manifests as excessive activity and endless movement, as well as hypokinesis, where a person becomes immobile or demonstrates slowed reactions. These manifestations may be accompanied by muscle rigidity, unusual postures, and refusal to follow any commands, making catatonia noticeable and sometimes frightening for those around.
In addition to motor disturbances, catatonic syndrome may also manifest in oculomotor disorders, perception disturbances, and mood changes. For example, a patient may experience deep depression as well as stupor, during which they may remain in one position for an extended period. This condition can arise as a consequence of various mental disorders, including schizophrenia and manic-depressive psychosis, as well as due to somatic diseases or intoxication. It is important to note that catatonic symptoms can vary in severity and duration, making their diagnosis and treatment a challenging task.
Diseases
Catatonic syndrome is a complex clinical condition that can manifest within various mental disorders and severe illnesses. Most often, catatonia is observed in schizophrenia, where it can be part of the symptomatic complex. Additionally, catatonia may develop as a result of illnesses such as severe depression, bipolar disorder, and even certain neurological disorders. This wide variability can complicate diagnosis, so it is important to consider the entire clinical picture of the patient.
The diseases associated with catatonic syndrome include:
- Schizophrenia
- Depressive disorders
- Bipolar disorder
- Neuroleptic malignant syndrome
- Autoimmune diseases, such as anti-NMDA receptor encephalitis
- Cerebrovascular diseases
- Toxic conditions (e.g., following drug or alcohol use)
It is important to remember that catatonic syndrome requires a comprehensive approach to treatment and psychiatric care, as its symptoms can range from postural immobility to extreme motor activity. Consulting qualified mental health professionals is a prerequisite for the successful treatment and recovery of the patient.
Diagnosis
The diagnosis of catatonic syndrome is a multi-step process that includes both clinical and laboratory methods. The psychiatrist or neurologist first conducts a detailed interview with the patient and their relatives to identify symptoms and their duration. It is important to rule out other conditions that may have similar manifestations, such as schizophrenia or depression. The collection of history may also include information about previous mental disorders and medications the patient may have taken.
In the next stage, the diagnosis may include the use of various laboratory tests and instrumental studies. This may involve blood tests that allow for the assessment of the patient’s overall condition and the exclusion of organic causes of catatonia, such as infections or metabolic disorders. Additionally, an EEG or MRI of the brain may be recommended to rule out neurological diseases. It is important for the diagnosis to be comprehensive, as catatonic syndrome can manifest within various psychiatric dysfunctions.
- Clinical examination and history taking
- Laboratory tests (blood test, urine test)
- Neuropsychological testing
- Electroencephalography (EEG)
- Magnetic resonance imaging (MRI)
- Consultation with other specialists (neurologist, therapist)
Which doctor to consult
Catatonic syndrome requires highly qualified medical assistance, and it is important to correctly identify the doctor to approach for diagnosis and treatment. First of all, patients should schedule an appointment with a psychiatrist. This specialist has the necessary knowledge about mental disorders and will be able to assess the clinical manifestations of the syndrome, as well as prescribe appropriate tests and therapy.
In some cases, a consultation with other doctors may also be needed, such as a neurologist, who will conduct further examinations, including neuroimaging, to rule out organic brain diseases. It will also be helpful to consult a therapist, who can assess the patient’s overall condition and prescribe tests to exclude somatic diseases that may cause or exacerbate the symptoms of catatonia.
- Psychiatrist
- Neurologist
- Therapist
- Psychotherapist
- Mental health social worker
Types of Catatonic Syndrome
Catatonic syndrome can manifest in various forms and have many variations, which depend on the characteristics of the underlying disease that causes this condition. The main types of catatonia include mutism, catalepsy, extrapolation, and other specific subtypes. Each of these types is characterized by unique symptoms and manifestations that assist doctors in diagnosing and choosing the most appropriate treatment.
Mutism, for example, is expressed as a complete absence of speech activity, even though the patient may be in a conscious state. Catalepsy is accompanied by excessive mobility and activity, while extrapolation manifests in purposeful and unusual actions by the patient. Understanding the different types of catatonic syndrome is an important aspect for the successful diagnosis and therapy of this condition.
- Mutism
- Catalepsy
- Extrapolation
- Catatonic excitement
- Prolonged catatonia
- Motor retardation
Causes of Catatonic Syndrome
Catatonic syndrome is a complex psychomotor disorder that can arise in patients for various reasons. The primary cause of catatonia is often the presence of mental illnesses, such as schizophrenia, exacerbation of bipolar disorder, or depression. In these cases, catatonia may manifest as a symptom of the underlying disorder, which requires a specialized approach to treatment and diagnosis.
However, catatonic syndrome can also be triggered by non-mental illnesses. For example, neurological disorders, such as cerebral stroke, tumors, or brain injuries, can play a significant role. In rare cases, catatonia may develop due to the influence of certain medications, toxic substances, or withdrawal from drugs, which requires immediate medical intervention.
- Schizophrenia
- Bipolar disorder
- Depression
- Cerebral stroke
- Brain tumors
- Neurological disorders
- Medication intoxication
Common Related Pathologies
Catatonic syndrome can occur not only as an independent disorder but also in conjunction with other mental and neurological diseases. It is important to note that its manifestations can vary significantly depending on the underlying diagnosis. One of the most common pathologies is schizophrenia, where catatonia is one of the forms of manifestation. In such cases, catatonic syndrome can lead to a significant deterioration in the patient’s condition and complicate the course of the illness.
Furthermore, catatonia may be observed in bipolar disorder, where characteristic manifestations of this form arise during periods of mania or depression. The syndrome can also be associated with organic psychoses, strokes, and severe neurodegenerative diseases such as Parkinson’s disease. Understanding the connections between catatonic syndrome and other diseases is essential for accurate diagnosis and the selection of effective treatment methods.
- Schizophrenia
- Bipolar disorder
- Organic psychoses
- Parkinson’s disease
- Depressive disorders
Expert Opinion
Catatonic syndrome is a serious neuropsychiatric disorder that can arise against the backdrop of various diseases, including schizophrenia, depression, and organic brain disorders. The presence of diverse symptoms such as stupor, mutism, excitation, as well as distinctive movement disorders, makes the diagnosis and treatment of this syndrome particularly challenging tasks. Experts emphasize that early detection and adequate therapy of catatonic syndrome significantly impact the prognosis and perception of the patient’s overall condition.
Given the multifactorial nature of this syndrome, it is important to adopt a comprehensive approach to treatment, which may include both medications and psychotherapeutic methods. The views of clinical psychiatry experts highlight the necessity for an individualized approach for each patient: the choice of treatment strategy is generally determined by existing comorbidities and the characteristics of the clinical picture. Openness and interaction between the doctor and the patient can significantly enhance the effectiveness of the treatment conducted and minimize the risk of relapses.

Treatment of Catatonic Syndrome
The treatment of catatonic syndrome requires a comprehensive approach and should be based on the individual characteristics of the patient. Typically, therapy includes both pharmacological and non-pharmacological methods. An important step in treatment is the identification and elimination of factors contributing to the development of the syndrome, such as stress, infectious diseases, or other mental disorders. Psychotherapy, including cognitive-behavioral techniques, can be helpful for patients suffering from catatonia, allowing them to cope with anxiety and restore psychological resilience.
Pharmacological therapy may include the use of antipsychotic medications, such as aminazine or risperidone, which help reduce the symptoms of catatonia. In some cases, benzodiazepines are also used, which alleviate anxiety and tension. Psychiatric assistance, especially in inpatient settings, is often necessary for monitoring the patient’s condition and selecting the most effective medications.
- Antipsychotic medications (e.g., aminazine, risperidone)
- Benzodiazepines (e.g., diazepam)
- Psychotherapy (individual and group)
- Supportive therapy (emotional support and social skills)
- Treatment of comorbid conditions (if any)
Complications
Catatonic syndrome can have serious health consequences if not diagnosed and treated in a timely manner. One of the main complications is physical problems that may arise due to the patient’s prolonged immobile state. For example, with prolonged immobilization, there is a possibility of developing deep vein thrombophlebitis, bedsores, or even muscle atrophy. These conditions require special medical intervention and monitoring by medical professionals.
In addition, emotional and psychological complications can also arise as a result of catatonia. Patients suffering from this syndrome may experience a high level of anxiety, depression, or even suicidal thoughts after emerging from a catatonic state. These psychological complications can lead to long-term dysfunction requiring long-term therapy and psychological support. Therefore, it is important not only for the physical recovery but also for the psychological recovery of the patient after experiencing catatonia.
- Deep vein thrombophlebitis
- Bedsores
- Muscle atrophy
- Psychiatric disorders
- Depression
- Anxiety states
- Suicidal thoughts