Vulvar neoplasms: symptoms, diagnosis, and treatment
About the symptom
New formations of the vulva can manifest various symptoms, which often depend on their nature and stage of development. At early stages, patients may not experience any discomfort, making early diagnosis difficult. However, with the progression of tumor processes, more pronounced symptoms may appear, such as itching, burning, pain, or discomfort in the vulvar area. These sensations may be accompanied by changes in the skin: the appearance of redness, swelling, or ulcers, which require the attention of a specialist.
Additionally, some women may notice the appearance of new formations in the form of lumps or thickening on the vulva. Such changes can be either benign or malignant, making thorough diagnosis necessary. It is important to pay attention to possible vaginal discharge that may have an unusual color or odor. If the above symptoms appear, it is strongly recommended to consult a gynecologist for diagnosis and necessary treatment, as timely intervention can significantly increase the chances of successful recovery.
Diseases
Neoplasms of the vulva can be either benign or malignant. Benign formations often present as tumors, cysts, or papillomas, which may not cause any symptoms or discomfort. However, in some cases, they can lead to itching, burning, or a feeling of pressure in the vulvar area. Malignant neoplasms, on the other hand, may have more serious symptoms, such as ulcers, bleeding, or changes in color and shape of the skin in the genital area. Early detection and diagnosis are critical for successful treatment, so it is important to regularly undergo preventive check-ups with a specialist.
Common diseases associated with vulvar neoplasms include:
- Vulvar neoplasia (dysplasia)
- Vulvar melanoma
- Human papillomavirus infection (warts and condylomas)
- Lipomas
- Vulvar adenoma
- Vulvar cysts (e.g., Gartner’s cysts)
- Keratosis
- Vulvar cancer
Consulting a specialist at the first signs or symptoms of vulvar neoplasms will help avoid complications and choose the optimal treatment strategy.
Diagnosis
The diagnosis of vulvar neoplasms is an important step in determining the nature and characteristics of pathological changes. Since symptoms may vary from mild discomfort to severe disturbances, the doctor usually begins with a detailed history-taking and clinical examination. A visual assessment of the vulva allows for the identification of the presence of a mass, its size, shape, and color, which serves as the basis for further investigation.
For more detailed analysis and confirmation of the diagnosis, additional examinations may be required. This typically includes laboratory tests such as cytology and biopsy. If necessary, more complex diagnostic methods may be applied, such as ultrasound and magnetic resonance imaging, which help to exclude the possibilities of malignant processes and other concomitant pathologies.
List of diagnostic services:
- Visual examination
- Cytology
- Biopsy
- Ultrasound examination (US)
- Magnetic resonance imaging (MRI)
- Histological examination
- Clinical blood tests
- Oncomarkers test
Which doctor to consult
When new formations on the vulva arise, it is extremely important to seek medical help as soon as possible. Initially, it is advisable to visit a gynecologist who specializes in diseases of the female reproductive system. The gynecologist will conduct an initial examination, collect medical history, and if necessary, refer you to a more specialized doctor, such as a dermatologist or an oncologist. These doctors have experience in diagnosing and treating conditions related to vulvar formations, which is especially important for choosing the right treatment method.
Modern medicine offers a wide range of diagnostic and therapeutic services for women experiencing problems with vulvar formations. Qualified specialists can help not only determine the nature of the formation but also suggest appropriate therapy options. If necessary, surgical intervention may be prescribed, as well as various methods of condition correction using medications. It is important not to postpone a visit to the doctor, as early diagnosis and intervention can significantly increase the chances of successful recovery.
- Gynecologist
- Dermatologist
- Oncologist
- Mammologist
- Psychologist (if psycho-emotional support is needed)
Types of Vulvar Neoplasms
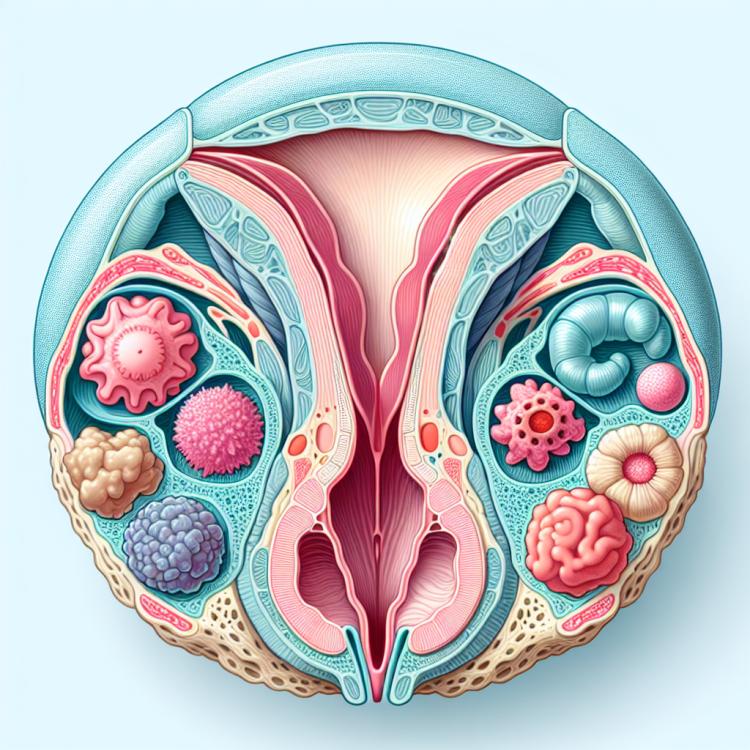
Vulvar neoplasms can originate in various ways and take different forms, making their classification important for accurate diagnosis and subsequent treatment. The main types of neoplasms include benign tumors, which are generally not a threat to health but can cause discomfort or cosmetic issues. These include, for example, papillomas, fibromas, and dermatofibromas. There is also a group of malignant neoplasms, such as vulvar melanoma and carcinoma, which require immediate intervention and serious treatment.
Another important category is precancerous conditions, which can gradually transform into malignant forms. These include dyskeratosis, leukoplakia, and vulvar neoplasia. These conditions require careful monitoring and often necessitate a biopsy to confirm the diagnosis.
- Benign tumors:
- papillomas
- fibromas
- dermatofibromas
- Malignant tumors:
- vulvar melanoma
- vulvar carcinoma
- Precancerous conditions:
- dyskeratosis
- leukoplakia
- vulvar neoplasia
Causes of Vulvar Neoplasms
Vulvar neoplasms may be caused by a multitude of factors, which include both genetic predispositions and external influences. One of the main reasons is the disruption of hormonal balance in the body, which can lead to the appearance of various tumors, both benign and malignant. For example, changes in the levels of estrogens and prostaglandins can broaden the spectrum of cellular changes, leading to the formation of neoplasms.
Moreover, infectious agents such as human papillomavirus (HPV) also play a significant role in the occurrence of neoplasms. HPV, particularly types 16 and 18, are associated with various types of cancer, including vulvar cancer. Various inflammatory processes that are chronic in nature may also act as a catalyst for changes in cellular structure, leading to the formation of neoplasms.
- Hormonal changes
- Infections (e.g., HPV)
- Chronic inflammatory processes
- Exposure to toxic substances
- Genetic predisposition
Common Associated Pathologies
Vulvar neoplasms can not only cause specific symptoms but also be associated with a number of other diseases and conditions. This underscores the importance of a comprehensive approach to the diagnosis and treatment of gynecological diseases. Regular medical examinations help identify accompanying pathologies at early stages, significantly increasing the chances of successful treatment.
Among the common associated pathologies are sexually transmitted infections (STIs) such as herpes, papillomavirus, and chlamydia. These infections can contribute to the development of vulvar neoplasms by negatively affecting the body’s immune response and creating favorable conditions for their development. It is also important to note that some benign tumors may arise against the background of venereal diseases, requiring careful monitoring and appropriate treatment.
- Sexually transmitted infections (STIs)
- Endometriosis
- Hormonal imbalance issues (e.g., polycystic ovary syndrome)
- Allergic reactions and dermatitis
- Thyroid diseases
Expert Opinion
Neoplasms of the vulva can be quite diverse and lead to various physical and emotional discomforts. Specialists emphasize the importance of timely diagnosis and treatment of such conditions, as some neoplasms may have precancerous or cancerous characteristics. An oncologist or dermatovenerologist are the specialists to consult at the first suspicion of pathologies in the vulva area. Especially since modern medicine offers a wide range of diagnostic methods, including biopsy and ultrasound examination, which allows for an accurate diagnosis and the appointment of optimal treatment.
According to experts, the main focus should be on changes in the skin condition, rashes, or growths that may appear on the vulva. These symptoms may be associated not only with neoplasms but also with infectious diseases or allergic reactions. Therefore, it is important not to ignore even minor changes and to undergo regular check-ups with a gynecologist.

Treatment of Vulvar Neoplasms
The treatment of vulvar neoplasms depends on their type, size, location, and the presence of symptoms. It is essential to conduct a thorough diagnosis to determine whether the neoplasm is benign or malignant. For benign neoplasms, such as cystic formations or papillomas, observation or minimally invasive procedures may be recommended to prevent their progression or remove them. Malignant neoplasms require a more comprehensive approach, which includes surgery, chemotherapy, or radiotherapy.
The primary goal of treatment is to alleviate symptoms and prevent the progression of the disease. In some cases, a combination of methods may be necessary, including surgery to remove the neoplasm, followed by additional treatment to prevent recurrence. Professional support and an individualized approach to the patient play a key role in the successful treatment process.
Main Treatment Methods:
- Surgical removal of the neoplasm
- Laser therapy
- Cryotherapy
- Chemotherapy (for malignant formations)
- Radiotherapy (if necessary)
- Regular monitoring and patient condition control
Complications
Neoplasms of the vulva can lead to various complications that significantly affect the patient’s quality of life. One of the most common complications is an infection resulting from damage to the skin or mucous membrane, which facilitates the entry of pathogenic microorganisms. This infection can be either local or systemic, requiring immediate medical intervention.
Other possible complications include recurrence of the neoplasms, which may require prolonged monitoring and repeat treatment. Unconventional or ineffective treatment methods can also lead to complications such as bleeding or scarring, which can further negatively impact the functionality of the vulva. In addition, chronic pain and discomfort become constant companions, making daily activities difficult and worsening the psychological and emotional state of patients.
- Infection at the site of the neoplasm
- Recurrence of neoplasms
- Chronic pain and discomfort
- Bleeding
- Formation of scars or tissue deformities