Pustules: Causes, Symptoms, Diagnosis, and Treatment
About the symptom
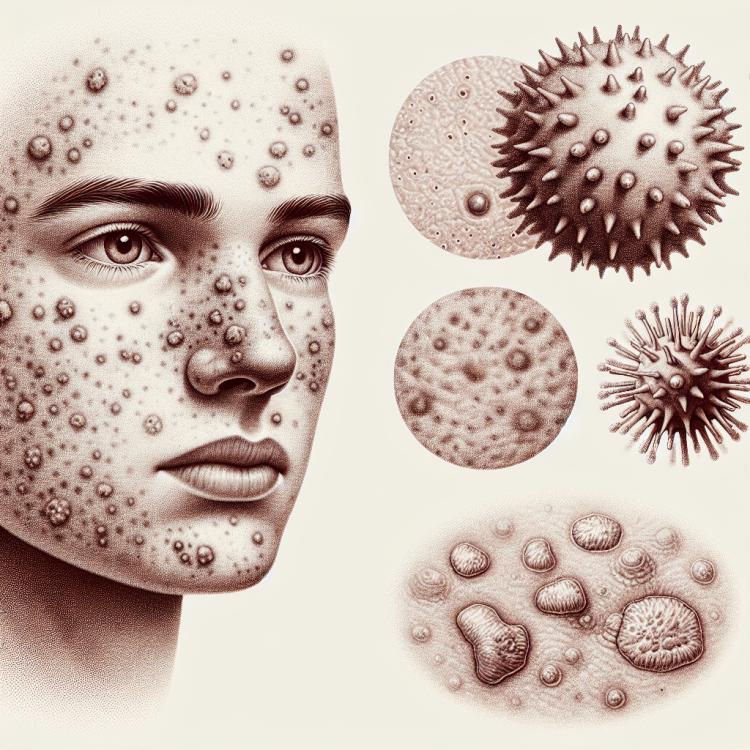
Pustules are small inflammatory lesions on the skin filled with fluid, usually with purulent content. They can appear on various areas of the skin and indicate the presence of inflammatory processes resulting from infections, allergic reactions, or other pathologies. Pustules are often associated with conditions such as acne, eczema, psoriasis, and many other skin diseases, making them an important diagnostic sign for specialists in dermatology.
Pustules may be accompanied by a range of other symptoms, including redness, itching, and tenderness in the area of inflammation. In some cases, they may occur in combination with other skin manifestations, such as papules or crusts. When pustules are present, it is important not to ignore their appearance, as this may indicate the need for diagnosis and commencement of treatment. Early consultation with a medical professional will help establish the cause of their occurrence and prevent possible complications, such as secondary infection or the spread of the inflammatory process to adjacent areas of the skin.
Diseases
Pustules are collections of fluid or pus that can occur on the skin as a result of various diseases. They are a serious symptom indicating inflammatory processes, infections, or other pathologies. For adequate diagnosis and subsequent treatment, it is crucial to determine the cause of pustule formation, as treatment will vary depending on the underlying disease.
The most common diseases that can cause pustules include:
- Acne – a condition that arises from clogged pores, leading to inflammation and the formation of pustules.
- Piodermatitis – a skin infection caused by bacteria, resulting in purulent inflammation and pustules.
- Scleroderma – an autoimmune disease where pustules may form due to changes in connective tissue.
- Folliculitis – inflammation of hair follicles, which may be accompanied by the formation of purulent pustules.
- Herpetiform dermatitis – a viral disease that manifests as blisters and pustules on the skin.
Each of these diseases requires careful attention and professional medical help to choose the optimal treatment strategy and prevent recurrences.
Diagnosis
The diagnosis of pustules, as well as other skin symptoms, begins with a thorough clinical examination. It is important to consider not only the appearance of the pustules but also accompanying symptoms such as redness, itching, or tenderness in the affected area. The doctor may perform a visual inspection to determine the nature of the rashes, their number, and location. More accurate diagnosis may require laboratory tests, such as skin analysis or a swab from the pustule to rule out an infectious process.
In addition, the patient’s medical history, health status, and possible allergies also play an important role in the diagnosis. Based on the collected information, the doctor may prescribe necessary examinations to determine the cause of the pustules’ appearance and identify the best treatment method. In some cases, a consultation with a dermatologist or an infectious disease specialist may be required for a deeper assessment of the patient’s condition.
List of diagnostic services:
- Visual examination of the skin
- Swab from the pustule for bacteriological examination
- Skin allergy tests
- Complete blood count
- Specific serological tests
- Dermatoscopy
Which doctor to see
If pustules appear on the skin, it is necessary to consult a doctor for diagnosis and appropriate treatment. Pustules can be a symptom of various conditions, from infections to allergic reactions, so it is important to understand which medical specialist to turn to. Usually, the initial stage of diagnosis may include a consultation with a dermatologist, who will assess the condition of the skin and suggest further research or treatment.
In some cases, the involvement of other specialists may be required, especially if a systemic disease or infection is suspected. For example, if a bacterial infection is suspected, a consultation with an infectious disease specialist may be necessary. Also, if the pustules are accompanied by other systemic symptoms such as high fever or general weakness, an examination by a therapist may be needed to rule out serious diseases.
Medical directions for treating the symptom:
- Dermatology
- Infectious diseases
- Allergology
- Immunology
- Therapy
Types of Pustules
Pustules are inflammatory formations that contain pus and occur on the skin or mucous membranes. They can vary depending on their origin and nature. Firstly, pustules can be divided into two main types: primary and secondary. Primary pustules arise as a result of inflammatory processes, such as acne, and represent the initial elements of skin lesions. Secondary pustules are a consequence of other diseases and may appear at the site of previously existing skin damage.
There are several clinical forms of pustules, each with its own features and causes. For example, pustules can result from bacterial infections, such as impetigo, or viral diseases, such as smallpox. It is important to note that pustules can differ in size, color, and degree of inflammation, which is also a significant factor for diagnosis and treatment. The classification of pustules helps doctors more accurately determine the sources of the problem and choose an appropriate treatment method.
- Pustules in acne
- Pustules due to bacterial infections
- Pustules in viral infections
- Pustules in fungal infections
- Allergic pustules (e.g., contact dermatitis)
Causes of Pustules
Pustules are small formations filled with fluid or pus that can arise from various causes. One of the main reasons for the appearance of pustules is an infection caused by bacteria, viruses, or fungi. The most common infections that lead to the formation of pustules include bacterial skin infections, such as impetigo, as well as viral infections, such as chickenpox.
Other factors that contribute to the formation of pustules may include inflammatory processes, allergic reactions, or autoimmune diseases such as psoriasis. Additionally, nerve and hormonal changes, stress, and poor nutrition can affect skin condition, potentially leading to the occurrence of pustules. It is important to consider that pustules may be a symptom of more serious illnesses, so consulting a specialist to determine the exact cause of their appearance would be a prudent step.
- Infectious diseases (e.g., ringworm, chickenpox)
- Allergic reactions (e.g., contact dermatitis)
- Autoimmune diseases (increased immune system activity)
- Skin injuries (e.g., cuts, insect bites)
- Hormonal changes (e.g., acne related to puberty)
Common Associated Pathologies
Pustules can be a symptom of various diseases and conditions that can vary greatly in nature. Most often, pustules arise as a result of infection, inflammation, or the body’s reaction to irritants. Pathologies associated with pustules can affect the skin and internal organs, causing concern among patients and requiring careful diagnosis and treatment.
Some of the most common diseases manifested by pustules include infections caused by microbes, viruses, or fungi. Additionally, pustules can occur in various dermatological conditions, such as acne, boils, and impetigo, which require medical intervention to prevent more serious complications. It is important to note that pustules can also appear in allergic reactions or in the presence of systemic diseases such as eczema or psoriasis.
- Acne
- Impetigo
- Boils
- Psoriasis
- Eczema
- Dermatitis
- Cutaneous candidiasis
- Syphilis
Expert Opinion
Pustules are inflammatory formations filled with purulent contents and can be indicative of various skin diseases. Skin experts note that pustules, while being an integral part of many conditions such as acne or dermatitis, should not be ignored. Their presence often indicates an infection or allergic reaction, which requires careful diagnosis and treatment.
Professionals strongly recommend against self-treatment, as incorrect application of remedies may worsen the skin condition. The best approach to pustules is to consult a dermatologist who can determine the exact cause and prescribe the necessary treatment. A qualified specialist can also provide skincare recommendations to help prevent recurrences and improve overall skin condition.
Finally, it is important to remember that pustules can occur not only on the face but also on other parts of the body. This makes a doctor’s examination even more important to rule out any hidden pathology and ensure proper therapy.

Treatment of Pustules
The treatment of pustules depends on their cause and severity. Pustules can appear on the skin as a result of various diseases and conditions, such as acne, infectious diseases, or allergic reactions. It is important to correctly identify the source of their appearance to avoid recurrent rashes. For this, it is necessary to consult a doctor who can prescribe the necessary tests and examinations.
In most cases, the treatment of pustules includes both local and systemic methods. Local remedies, such as antiseptic and anti-inflammatory creams, can help reduce inflammation and speed up healing. If pustules are caused by an infection, antibiotic therapy or antifungal medications may be required. It is also important to observe personal hygiene rules and avoid damaging the skin.
The most common methods for treating pustules include:
- Antibiotics (for bacterial infections)
- Anti-inflammatory medications
- Topical antiseptics
- Hormonal medications (for hormonal disorders)
- Physiotherapy procedures
Complications
Pustules are a type of skin rash that can manifest on various areas of the body and be caused by a multitude of factors. Depending on the reason for the appearance of pustules, they can lead to various complications, both physical and psycho-emotional. One of the main risks is the possibility of secondary bacterial infection, which can cause serious inflammatory processes in the skin and underlying tissues, in turn requiring more serious medical intervention.
Furthermore, the presence of pustules can lead to the formation of scars and hyperpigmentation, especially if the rashes are located in areas where the skin is subject to mechanical stress or friction. Since skin issues are visible, they can cause psycho-emotional complications such as reduced self-esteem, anxiety, and even depression, which also requires attention from specialists.
- Secondary bacterial infections
- Scars and marks on the skin
- Hyperpigmentation
- Dermatitis
- Psycho-emotional disorders