Vaginal prolapse: causes, symptoms, and treatment
About the symptom
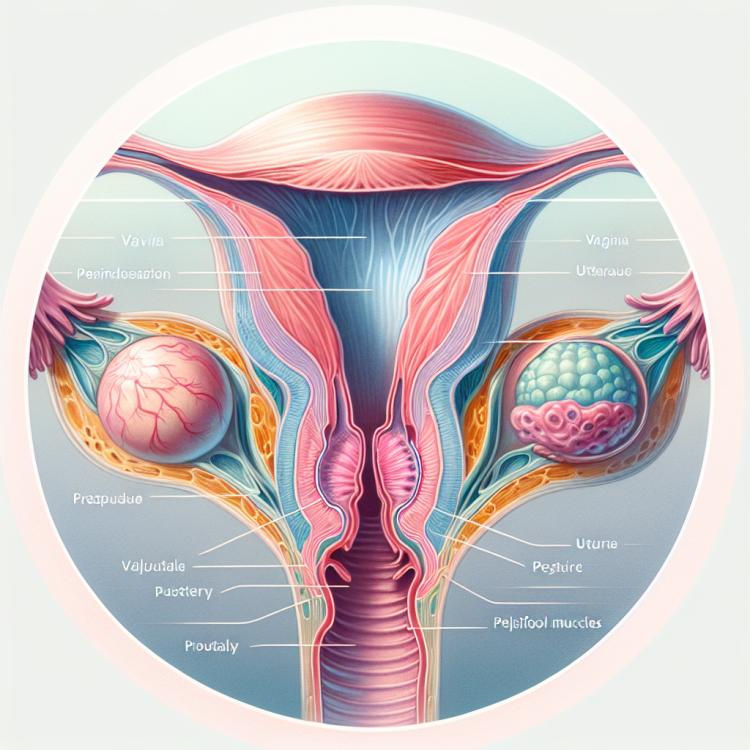
Prolapse of the vagina, or vaginal prolapse, is a condition in which the vagina descends and moves downward beyond its normal position. This occurs as a result of weakening of the muscles and tissues that support the pelvic organs. The main symptoms of this condition include a feeling of heaviness or pressure in the pelvic area, discomfort during physical activity, as well as the appearance of protruding tissues from the vagina. Women may also experience problems with urination, including incontinence or difficulty emptying the bladder.
In addition, women suffering from vaginal prolapse may experience changes in sexual function, including pain or discomfort during intercourse. These symptoms can vary in intensity depending on the stage of the condition and the woman’s level of physical activity. It is important to note that many women may not report their symptoms due to shame or fear; however, timely consultation with a doctor can help avoid further complications and improve quality of life.
Diseases
Vaginal prolapse may be associated with several diseases and conditions that contribute to the deterioration of pelvic floor health. Among them are conditions like chronic constipation, which leads to increased pressure in the abdominal cavity, as well as heavy physical exertion, such as lifting weights. These factors can contribute to the development of vaginal prolapse, which in turn requires medical intervention.
Other diseases associated with vaginal prolapse include certain hormonal disorders, such as estrogen deficiency during menopause, which leads to weakening of tissues and ligaments. Women who have given birth multiple times also have an increased risk of developing this condition due to excessive stretching and damage to pelvic floor muscles. Without proper attention to these conditions, the disease may progress, affecting the quality of life of the woman.
- Vaginal prolapse
- Joint hypermobility syndrome
- Hormonal disorders (in particular, estrogen deficiency)
- Chronic constipation
- Atrophic vaginitis
- Lack of physical activity
- Urinary and sexual function disorders
Diagnosis
Diagnosing vaginal prolapse is an important step in determining the degree and cause of this condition. The doctor, usually a gynecologist, conducts a thorough medical examination, including taking a medical history to understand when and how the symptoms arose, as well as other factors that may have influenced the development of the problem. Aspects such as childbirth, age, presence of chronic diseases, and the patient’s lifestyle may be considered during the examination process.
After gathering information, a physical examination is performed, during which the doctor will assess the vaginal and pelvic area. In some cases, additional tests may be required to confirm the diagnosis. For example, ultrasound imaging or a special examination – cystometry – may be prescribed to assess bladder function and identify potential coexisting issues.
List of Diagnostic Services
- General clinical examination
- Gynecological examination
- Ultrasound examination of the pelvic organs
- Cystometry
- Tests for infection detection
- MRI or CT of the pelvic organs
- Laboratory tests (complete blood count, hormone tests, etc.)
Which doctor to consult
When symptoms related to vaginal prolapse appear, it is important not to delay a visit to a medical specialist. The first step is a consultation with a gynecologist, who has sufficient knowledge and experience to diagnose such a condition. The doctor will conduct a primary examination, gather a medical history, and, if necessary, refer for additional tests. The gynecologist will help determine the extent of the problem and develop an individual treatment plan.
If more specialized assistance is needed, the gynecologist may recommend consulting other specialists. For example, in cases where surgical intervention is required, a consultation with a urogynecologist may be necessary. These specialists deal with diseases of the urogenital system and can offer modern methods for correcting vaginal prolapse, including minimally invasive surgeries.
List of medical specialties for treatment:
- Gynecology
- Urogynecology
- Physiotherapy
- Rehabilitation
- Psychology (for patient support)
Types of Vaginal Prolapse
Vaginal prolapse is a condition associated with the descent of vaginal structures due to weakening of the supportive tissues. There are several types of this condition, depending on the degree and direction of the prolapse. The first and most common type is direct vaginal prolapse, where the wall of the vagina descends into the pelvic cavity, which can lead to difficulties during intercourse and the emergence of other discomforting sensations.
Another type is the prolapse of the vaginal dome, which is more often seen in women after childbirth and may be associated with chromosomal anomalies or hormonal changes in the body. There is also a combined prolapse, where the descent of multiple structures occurs simultaneously: the walls of the vagina and the uterus. Each of these prolapses requires an individual approach to treatment, highlighting the importance of timely consultation with a specialist.
- Direct vaginal prolapse
- Prolapse of the vaginal dome
- Combined prolapse of the vagina and uterus
Causes of Vaginal Prolapse
Vaginal prolapse, or vaginal prolapse, is a condition in which the vagina shifts downward and may partially or completely extend beyond the external genitalia. This condition is most commonly seen in women who have given birth, but there are other predisposing factors as well. The primary cause of vaginal prolapse is the weakening of the pelvic support tissues, including ligaments and muscles, which can occur due to age, hormonal changes, and physical trauma.
Giving birth through natural childbirth, especially multiple births, subjects the pelvic tissues to significant stretching and trauma. Women over the age of 50, particularly after menopause when estrogen levels decline, are most at risk for this condition, as this also affects tissue elasticity. Additionally, increased intra-abdominal pressure, for example, due to obesity, chronic coughing, or constipation, can be another contributing factor to the development of vaginal prolapse.
- Connective tissue diseases
- Systemic diseases (e.g., diabetes)
- Surgical interventions in the pelvic organs
- Pelvic trauma
- Lifestyle factors (overeating, lack of physical activity)
Common Related Pathologies
Vaginal prolapse is not only an independent condition but also a state that is often associated with a number of other pathologies. These diseases can significantly exacerbate discomfort and symptoms, as well as affect the overall health of the patient. Therefore, it is important to understand which conditions may accompany vaginal prolapse.
One of the common related pathologies is uterine prolapse. This condition occurs when the muscles and ligaments supporting the uterus become weak, causing it to drop into the vaginal canal. Other common pathologies include cystocele (prolapse of the bladder), rectocele (prolapse of the rectum), and vaginal atrophy, which may occur due to changes in estrogen levels, especially after menopause.
- General pelvic organ prolapse
- Cystocele (bladder prolapse)
- Rectocele (rectal prolapse)
- Vaginal atrophy
- Mild to moderate forms of urinary incontinence
Expert Opinion
Vaginal prolapse is a serious problem that requires attention from both patients and medical professionals. Obstetrician-gynecologist Olga Ivanova emphasizes that this condition is often associated with age-related changes, childbirth, and other factors affecting women’s health. She notes that women often feel embarrassed to discuss this issue, which significantly complicates diagnosis and treatment.
According to the expert, an important step in combating vaginal prolapse is early diagnosis and timely consultation with a specialist. She recommends not to ignore symptoms such as discomfort, a feeling of heaviness, or “prolapse” in the pelvic area. The sooner treatment is initiated, the easier it will be to resolve the problem and restore quality of life. Olga Ivanova also highlights that there are effective prevention and therapy methods that can help avoid this condition, including physical activity and special exercises to strengthen the pelvic floor muscles.

Treatment of Vaginal Prolapse
The treatment of vaginal prolapse depends on the severity of the problem and can include both conservative and surgical methods. Conservative approaches involve the use of exercises aimed at strengthening the pelvic floor muscles, as well as the application of special underwear and vaginal support devices. Kegel exercises, aimed at strengthening the vaginal and perineal muscles, become particularly important for women suffering from this problem.
In cases where conservative methods are insufficiently effective, surgical treatment is resorted to. Surgical interventions can vary from minimally invasive procedures to more serious surgeries aimed at restoring the anatomy of the pelvic organs. It is important that the choice of treatment method is made in consultation with a medical specialist who can take into account the individual characteristics and health status of the patient.
- Exercises to strengthen pelvic floor muscles
- Vaginal support devices
- Surgical intervention (colpopexy, vaginal lift)
- Physical therapy
- Hormonal therapy
Complications
Vaginal prolapse can lead to a number of serious complications if medical attention is not sought and treatment is not initiated. One of the most common complications is chronic pelvic pain, which can arise from excessive stretching of the ligaments and muscles supporting the reproductive organs. This condition can significantly reduce a woman’s quality of life and lead to emotional and psychological issues.
Additionally, vaginal prolapse can result in urinary incontinence and constipation. Women with this condition may experience difficulties in controlling urination, which can lead to urinary tract infections. Prolonged neglect of health can also lead to fatty atrophic changes in tissues, which exacerbates the prolapse and creates additional complications during potential surgical interventions.
- Chronic pelvic pain
- Urinary incontinence
- Urinary tract infections
- Constipation
- Fatty atrophy of tissues