Ulcers on the oral mucosa: causes, symptoms, and treatment
About the Symptom
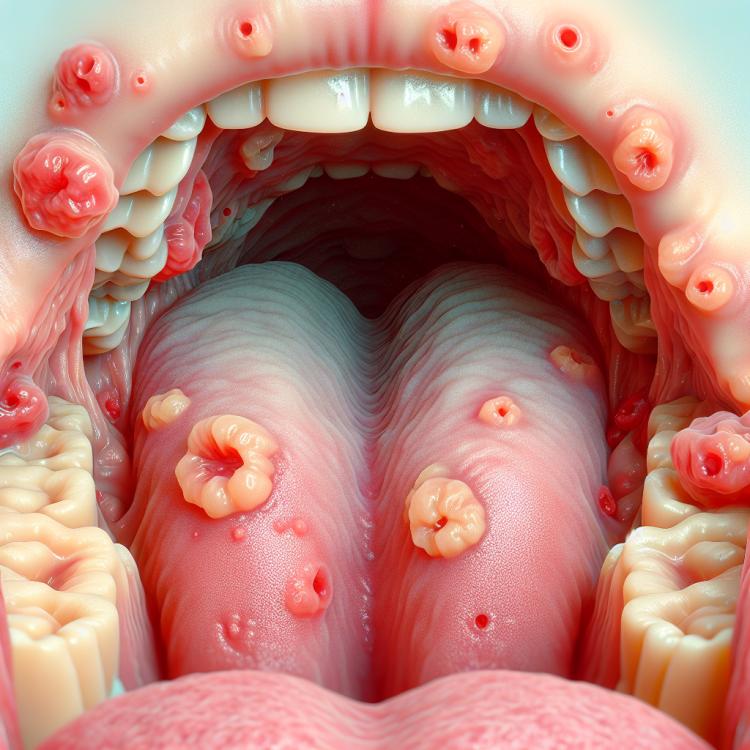
Sores on the oral mucosa are not only unpleasant but also a fairly common occurrence that many people face. These small, painful formations can appear on the lips, tongue, gums, and the inside of the cheeks, causing discomfort while eating, talking, and even at rest. The main causes of the appearance of sores can vary from minor injuries and irritations to more serious diseases, such as viral or bacterial infections. It is important to remember that such manifestations can signal the presence of internal disorders in the body, including allergic reactions or vitamin deficiencies.
Symptoms accompanying sores on the oral mucosa may include burning, itching, as well as increased sensitivity in the affected area. Some patients report the onset of itching and redness around the sore, and in more severe cases, signs of general intoxication may also occur — elevated temperature, weakness, and decreased appetite. If the sores do not resolve within a few days or are accompanied by other alarming symptoms, it is strongly recommended to consult a doctor to determine the exact cause of their appearance and to prescribe appropriate treatment.
Diseases
Ulcers on the oral mucosa can be a symptom of various diseases, from non-infectious to infectious. They can arise due to decreased immune function, food allergies, mechanical injuries, or as a reaction to stress. The most common diseases associated with ulcer formation include aphthous stomatitis, herpes infection, candidiasis, and others. Each of these diseases has its unique characteristics, making accurate diagnosis important for effective treatment.
Aphthous stomatitis, for example, is characterized by the appearance of painful ulcers on the mucosa, which can significantly hinder eating and speaking. Unlike this disease, herpes infection is accompanied by rashes of viral origin and can recur multiple times. Candidiasis, or oral thrush, develops as a result of fungal overgrowth, leading to the formation of whitish ulcers. Understanding the various diseases associated with ulcers allows for better preparation for a consultation with a specialist and obtaining the necessary help.
- Aphthous stomatitis
- Herpes infection
- Oral mucosal candidiasis
- Traumatic ulcer
- Leukoplakia
- Stevens-Johnson syndrome
- Behçet’s disease
- Psoriasis
Diagnosis
The diagnosis of sores on the oral mucosa requires a careful approach and may include several stages. Initially, the doctor conducts a detailed interview with the patient regarding the time of onset of the sores, their location, size, and the nature of the pain sensations. It is also important to find out whether the patient has had similar issues previously, the presence of chronic diseases, allergies, and medications being taken. This information can greatly assist in determining the possible causes of the sores.
After collecting the medical history, the doctor may perform a physical examination, which includes a visual inspection of the oral cavity. In some cases, additional studies may be required for a more accurate diagnosis, such as laboratory tests of saliva or a biopsy of tissues taken from the area of the sore. If necessary, a consultation with other specialists, such as a dentist or dermatologist, may be appointed for a more in-depth study of the problem.
- Complete blood count
- Test for infectious diseases (e.g., herpes or HIV)
- Biopsy of the sore
- Scraping from the surface of the sore for microscopic examination
- Allergy tests
- Consultation with a dentist
- Ultrasound examination to rule out diseases of internal organs
Which doctor to consult
If you have developed ulcers on the mucous membrane of the mouth, it is important to see a doctor in a timely manner for an accurate diagnosis and appropriate treatment. The most suitable specialist in this case is a dentist, who will examine the condition of the oral cavity, assess the nature of the ulcers, and may identify possible causes of their appearance. In some cases, if the dentist suspects the presence of systemic diseases, a consultation with narrow specialists, such as a dermatologist or a hematologist, may be required.
It is also important to remember that ulcers on the mucous membrane of the mouth can be a result of various diseases, and their treatment requires a comprehensive approach. When visiting a doctor, it is important to also report other symptoms you are observing so that the specialist can form a complete picture of your health condition and prescribe the necessary diagnostic procedures.
- Dentist
- Dermatologist
- Hematologist
- Therapist
- Allergist
Types of Ulcers on the Oral Mucosa
Ulcers on the oral mucosa can manifest in various forms and sizes, each possibly indicating different causes for their appearance. The most common types of ulcers are aphthous ulcers, which are small painful erosions that occur on the inner surface of the cheeks, lips, or tongue. These ulcers typically have a white or yellowish film and a red border, causing discomfort while eating and speaking.
Another type is herpetic ulcers, caused by the herpes virus. They often appear as clusters of small blisters that burst and turn into painful ulcers. It is also worth noting the ulcers associated with candidiasis, caused by fungi of the genus Candida, which may have a whitish coating and increase the likelihood of other infections.
- Aphthous ulcers
- Herpetic ulcers
- Ulcers caused by candidiasis
- Ulcers related to systemic diseases (e.g., in HIV or Crohn’s disease)
- Traumatic ulcers (after burns, mechanical injuries)
Causes of sores on the oral mucosa
Sores on the oral mucosa can occur for a number of reasons, ranging from infectious diseases to autoimmune disorders. One of the most common causes is viral infections, such as herpes or viruses that cause stomatitis. These viruses can lead to the formation of painful sores that make eating and speaking difficult.
In addition to viruses, sores can appear as a result of various allergic reactions to food, medications, or hygiene products. Autoimmune diseases, such as Behcet’s disease or gluten enteropathy, can also be a cause of sores. Finally, injuries and mechanical damage to the mucosa, for example, from sharp edges of teeth or ill-fitting dental prostheses, can contribute to the formation of sores.
- Viral infections (e.g., herpes, stomatitis)
- Bacterial infections (e.g., syphilis)
- Autoimmune diseases (e.g., Behcet’s disease)
- Allergic reactions
- Injuries to the oral mucosa
- Poor nutrition (vitamin deficiency)
- Stress and fatigue
Common Associated Pathologies
Ulcers on the oral mucosa can be a symptom of various diseases that affect not only the oral cavity but the entire body. These ulcers often arise as a result of general weakening of the immune system, infectious processes, or chronic diseases. The pathologies associated with the appearance of ulcers can range from mild to severe, requiring the involvement of multiple specialists for diagnosis and treatment.
Some of the common diseases that can lead to the formation of ulcers in the mouth include viral infections such as herpes or chickenpox, a range of chronic ailments, for example, Crohn’s disease, and various autoimmune conditions such as pemphigus. It is also essential to pay attention to the impact of systemic diseases, such as diabetes and HIV infection, which can negatively affect the condition of the oral mucosa and increase the likelihood of ulcer formation.
- Herpetic infection
- Candidiasis (thrush)
- Aphthous stomatitis
- Crohn’s disease
- Pemphigus
- Diathesis
- Vitamin B12 deficiency
- Diabetes
- HIV infection
Expert Opinion
Ulcers on the oral mucosa are a common problem faced by many patients. According to experts in the fields of dentistry and dermatology, the importance of correctly diagnosing the causes of these ulcers cannot be overstated. Some ulcers may result from simple injuries or infections, while others may signal serious systemic diseases such as Crohn’s disease or human papillomavirus infection. Therefore, consulting a specialist is critically important for selecting the right treatment method and preventing the recurrence of ulcers.
Experts also emphasize that ulcers on the oral mucosa can vary in shape and size, requiring an individualized approach to treatment. Short-term ulcers associated with mechanical damage or auto-trauma can be quickly resolved with local treatment, while chronic painful lesions often require more comprehensive medical intervention, including changes in diet and lifestyle. Since each case is unique, it is important to rely on the comments of experienced doctors who can help develop an effective action plan for the patient.

Treatment of ulcers on the oral mucosa
The treatment of ulcers on the oral mucosa depends on the cause of their occurrence and the severity of symptoms. Initially, it is important to consult a doctor for diagnosis and identification of the underlying disease. In some cases, ulcers may indicate serious illnesses such as stomatitis, herpes, or even sexually transmitted infections. Therefore, appropriate examination and medical prescription are essential.
At the initial stage of treatment, antiseptics may be used to prevent infections and accelerate healing. It is also important to maintain oral hygiene and avoid spicy, salty, and acidic foods that may worsen the condition. In some cases, analgesics and ointments are used to relieve pain. An important aspect is supporting the immune system through proper nutrition and vitamin supplementation, which also contributes to faster recovery.
- Antiseptics (rinses, gels)
- Pain relievers
- Antiviral medications (if necessary)
- Diet compliance (avoid irritating foods)
- Immunostimulants (vitamins and minerals)
Complications
Ulcers on the mucous membrane of the mouth can lead to a number of complications if necessary medical intervention is not received in time. Initially, even small ulcers can significantly worsen quality of life, causing pain and discomfort while eating and speaking. These symptoms may lead to a reluctance to eat, which in turn can result in weight loss and nutrient deficiencies.
Moreover, some ulcers may be a sign of more serious diseases, such as infections or autoimmune conditions. The use of improper treatment methods or ignoring symptoms can lead to a worsening of the condition and the development of chronic forms of diseases. Therefore, it is important not to self-diagnose or self-treat, but to consult a specialist for an accurate diagnosis and treatment recommendations.
- Loss of appetite and, consequently, weight loss
- Mucosal infections
- Chronic inflammatory processes
- Exacerbation of existing diseases (e.g., viral infections)
- Deterioration of psycho-emotional state due to constant pain