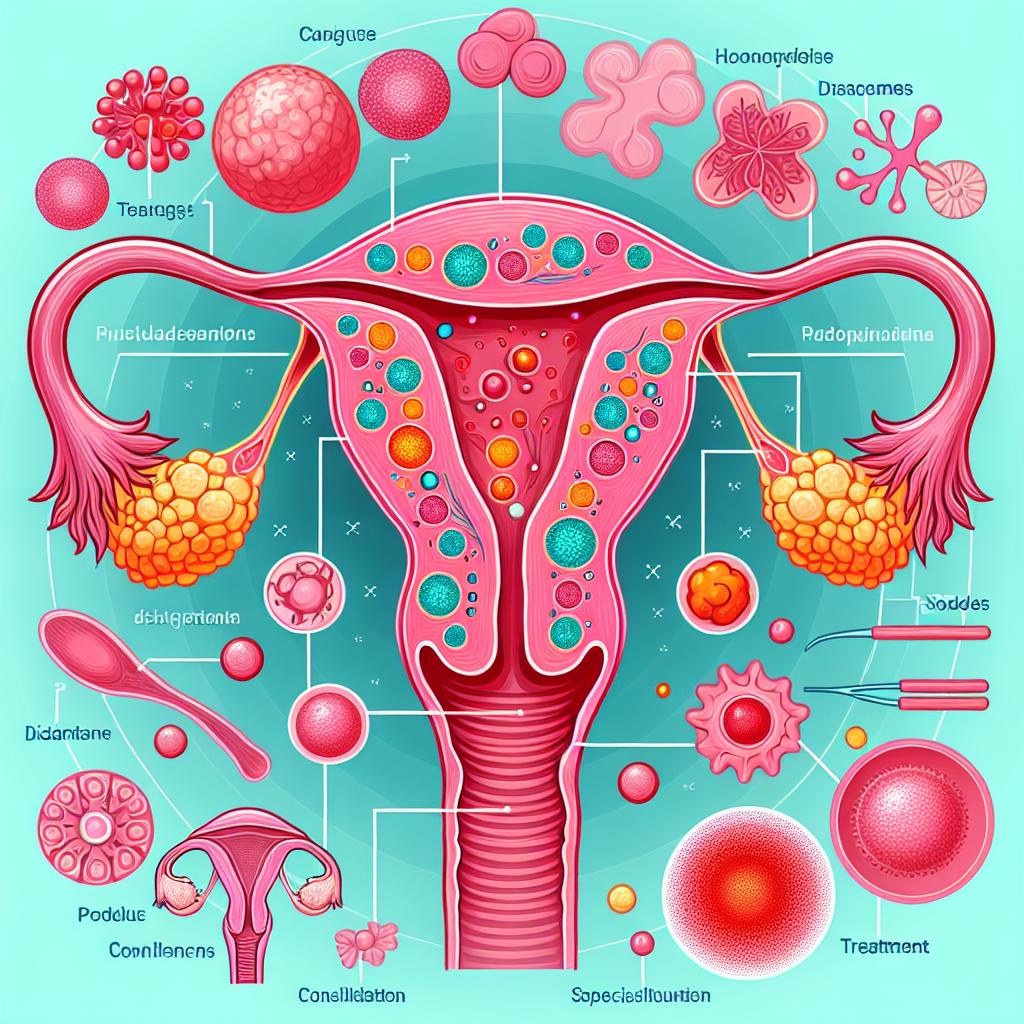
Adenomyosis of the uterus: diagnosis and modern treatment methods
- Fundamentals of uterine adenomyosis: understanding and diagnosis.
- Pathogenesis of uterine adenomyosis: main causes and risk factors.
- Main signs of uterine adenomyosis: how to recognize them.
- Effective approaches to the treatment of uterine adenomyosis: a look from specialists.
- Methods of diagnosing uterine adenomyosis: modern approaches.
- Modern approaches to the treatment of uterine adenomyosis.
- Measures for the prevention of uterine adenomyosis: disease prevention.
- Interesting aspects of uterine adenomyosis: amazing facts
- FAQ
Fundamentals of uterine adenomyosis: understanding and diagnosis.
Adenomyosis of the uterus is a pathological condition in which glandular cells of the endometrium invade the muscle layer of the uterus, causing changes and dysfunction. The diagnosis of this disease is based on clinical manifestations as well as imaging methods such as ultrasound, MRI, and histological examination of biopsy material after hysterectomy. Accurate and timely diagnosis of uterine adenomyosis is key to prescribing effective treatment and preventing possible complications.
Pathogenesis of uterine adenomyosis: main causes and risk factors.
Adenomyosis of the uterus has a multifactorial etiology, where estrogens play a key role. Estrogen levels in a woman’s body increase during life periods such as pregnancy, prolonged hormonal therapies, or obesity. This contributes to endometrial hyperplasia and the infiltration of endometrial cells into the muscular layer of the uterus. Other risk factors in the development of adenomyosis may include various uterine injuries, surgical interventions, immune system disorders, and genetic predispositions.
- Hormonal imbalance: increased levels of estrogens and decreased levels of progesterone contribute to the development of uterine adenomyosis.
- Genetic predisposition: having relatives with adenomyosis may increase the risk of developing this disease.
- Injuries and surgeries on the uterus: surgical interventions and injuries in the uterine area can promote the growth of endometrial cells into the muscle layer.
- Obesity: excess weight can lead to hormonal imbalance and create conditions for the development of adenomyosis.
- Uncontrolled use of hormonal medications: prolonged and irregular use of hormonal medications can have a negative impact on the endometrium and contribute to the development of the disease.
Main signs of uterine adenomyosis: how to recognize them.
Adenomyosis of the uterus can manifest with various symptoms, including heavy and painful menstruation, pain in the lower abdomen and pelvic area, as well as pain during sexual intercourse. Some patients may also experience irregular bleeding between periods and general fatigue. Diagnosing adenomyosis can be challenging due to the similarity with symptoms of other gynecological disorders, so it is important to consult a doctor for diagnosis if this condition is suspected.
- Heavy and painful menstruations: women with adenomyosis often experience increased volume and duration of menstruations, accompanied by severe pain.
- Pain in the lower abdomen and pelvic area: characteristic pain in the pelvic area can occur both during menstruation and at other times in the cycle.
- Pain during intercourse: dyspareunia, or painful intercourse, can be one of the symptoms of adenomyosis, caused by inflammation of the endometrium.
- Irregular bleeding: possible bleeding outside the menstrual cycle may be a sign of disorders caused by adenomyosis.
- General fatigue and malaise: women with adenomyosis often complain of fatigue and general weakness related to prolonged suffering from the symptoms of the disease.
Effective approaches to the treatment of uterine adenomyosis: a look from specialists.
Experts in the field of gynecology highlight several effective approaches to the treatment of uterine adenomyosis, including conservative methods, surgical intervention, and the latest treatment techniques. Conservative therapy often involves the use of hormonal medications, such as contraceptives, hormonal IUDs, and gonadotropin agonists, to reduce symptoms and halt the progression of the disease. Surgical treatment, such as hysterectomy or removal of affected tissue, may be recommended in cases of severe disease or lack of effectiveness of conservative therapy.
New treatment methods for adenomyosis, including focused ultrasound and drug therapy aimed at suppressing endometrial growth, are also discussed among specialists. Approaches to individualizing treatment, taking into account age, the desire to preserve fertility, the severity of symptoms, and other factors, are significant in making decisions about the optimal therapy strategy for uterine adenomyosis.

Methods of diagnosing uterine adenomyosis: modern approaches.
To diagnose adenomyosis of the uterus, modern medicine offers a number of effective methods, including ultrasound (US) using a vaginal transducer, which allows visualization of changes in the structure of the uterus. In addition, magnetic resonance imaging (MRI) provides a more accurate determination of the size and distribution of the affected areas of the uterus, which is important for diagnosis. Hysteroscopy, performed with the introduction of an optical instrument through the cervical canal, is another diagnostic method that allows the doctor to directly examine the uterine cavity and take a biopsy for laboratory tests to confirm the diagnosis.
Thanks to the development of modern diagnostic methods for adenomyosis of the uterus, specialists can make a more accurate and timely diagnosis, which contributes to the selection of the optimal treatment strategy. Studies show that the combination of various diagnostic methods, such as US, MRI, and hysteroscopy, improves the accuracy and reliability of diagnosing adenomyosis of the uterus, which significantly affects the effectiveness of treatment and the prognosis for patients.
- Ultrasound examination (US): Visualization of changes in the structure of the uterus using a vaginal transducer allows for the identification of possible lesions and changes in tissues.
- Magnetic resonance imaging (MRI): Detailed imaging of the size and structure of the uterus using MRI aids in determining the extent and location of the disease for further diagnostics.
- Hysteroscopy: A procedure that allows for direct examination of the uterine cavity using an optical instrument, which helps in diagnosis and biopsy collection.
- Laboratory blood tests: Investigating the levels of certain markers in the blood can be useful for assessing the degree of inflammation and other pathological processes associated with adenomyosis.
- Computed tomography (CT): The use of X-ray radiation to create 3D images of organs, including the uterus, can help in recognizing changes and structural anomalies.
Modern approaches to the treatment of uterine adenomyosis.
In cases where conservative treatment does not bring the desired effect or in cases of severe disease progression, surgical intervention may be required. Surgical methods, such as hysterectomy (removal of the uterus) or resection of the affected areas of the endometrium, may be recommended by doctors to improve the quality of life of patients and alleviate symptoms, especially in cases of significant dysfunctional bleeding and chronic pain.
- Conservative therapy: Includes the intake of hormonal medications, anti-gonadotropin agents, and medications aimed at improving the estrogen-progesterone balance.
- Medication treatment: The use of drugs such as non-steroidal anti-inflammatory drugs, analgesics, and antibiotics to relieve pain and inflammation in uterine adenomyosis.
- Surgical methods: Performing surgeries such as hysterectomy, endometrial resection, laparoscopic or hysteroscopic interventions to remove affected areas and improve the condition of the uterus.
- Minimally invasive procedures: The application of methods such as focused ultrasound and endovaginal microwave therapy for the treatment of adenomyosis without surgical intervention.
- Individualization of treatment: Determining a treatment strategy considering age, desire to preserve fertility, severity of symptoms, and overall condition of the patient to achieve the best results.
Measures for the prevention of uterine adenomyosis: disease prevention.
Regular visits to a gynecologist for screening and early detection of changes in the uterus also play a key role in the prevention of adenomyosis. Examinations such as ultrasound and hysteroscopy can help identify early stages of the disease, allowing for treatment to begin at an early stage. Specialists may also recommend maintaining a healthy lifestyle, regularly monitoring hormonal status, and timely management of other illnesses to reduce the risk of developing uterine adenomyosis.
- Maintaining a healthy lifestyle: Leading an active lifestyle, including regular physical exercise and healthy nutrition, helps maintain hormonal balance and the health of the uterus.
- Avoiding prolonged hormonal medications: Minimal use of hormonal medications without consulting a doctor helps prevent possible imbalances and risks of developing adenomyosis.
- Regular visits to the gynecologist: Conducting screening examinations and consultations with a specialist contribute to the early detection of changes in the uterus and timely initiation of treatment.
- Examinations to detect changes: Ultrasound, hysteroscopy, and other diagnostic methods help conduct follow-up examinations for the early detection of possible changes in the uterus.
- Maintaining regular monitoring of hormonal status: Under the guidance of a doctor, maintaining a stable hormonal status can help reduce the risk of developing uterine adenomyosis and other gynecological diseases.
Interesting aspects of uterine adenomyosis: amazing facts
Another interesting fact is that epidemiological studies show that adenomyosis of the uterus is more commonly found in women aged 40-50 years, although there is also a small percentage of cases where this disease may manifest in younger women. This underscores the importance of early diagnosis and preventive measures to monitor uterine health and initiate timely treatment.