Achalasia of the cardia: diagnosis, treatment, and prognosis
- Understanding Cardia Achalasia: Symptoms, Diagnosis, and Treatment
- Factors contributing to the development of Achalasia of the cardia
- Notable signs of Cardia Achalasia
- The professionals’ perspective on the therapy of cardia achalasia
- Checking and detecting Cardia Achalasia
- Principles of Therapy for Cardiac Achalasia
- Measures to prevent achalasia of the cardia
- Fascinating facts about Achalasia cardia
- FAQ
Understanding Cardia Achalasia: Symptoms, Diagnosis, and Treatment
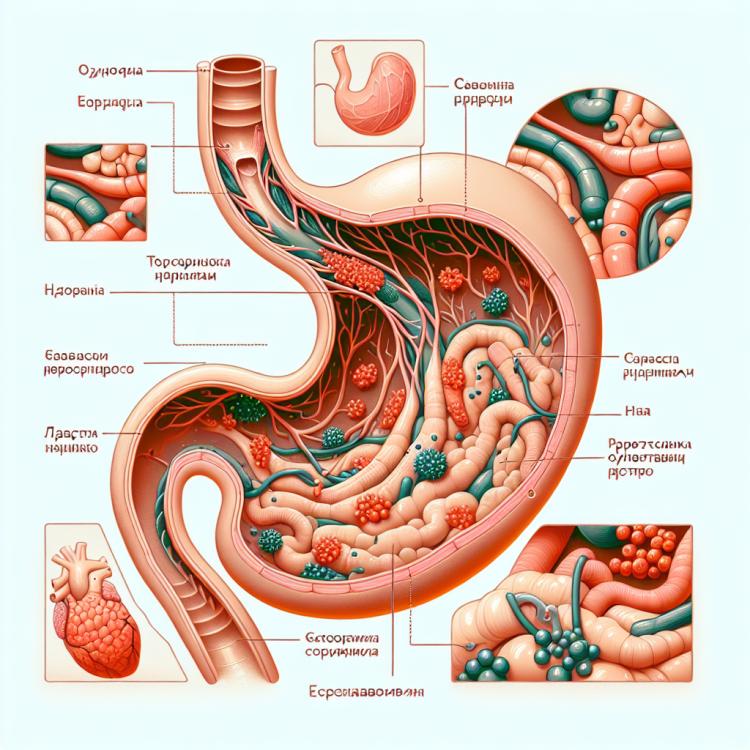
Achalasia of the cardia is a rare esophageal disease characterized by impaired peristalsis and the inability of the lower esophageal sphincter to close. Symptoms of achalasia include dysphagia, regurgitation, chest pain, often accompanied by vomiting and bloating. Diagnosis is performed using esophagogastroduodenoscopy, X-ray contrast study of the esophagus, manometry, and esophageal videomanometry.
Treatment for achalasia of the cardia focuses on alleviating symptoms and improving the patient’s quality of life. Treatment methods may include medication therapy, botulinum injection, pneumatic dilation, or surgical intervention. The choice of treatment method is based on the severity of achalasia symptoms, the overall health of the patient, and potential complications.
Factors contributing to the development of Achalasia of the cardia
Achalasia of the cardia is a rare esophageal disease characterized by impaired peristalsis and insufficient relaxation of the lower esophageal sphincter during swallowing. However, the exact causes of achalasia of the cardia remain not completely studied. A number of factors, including heredity, autoimmune and nerve imbalance, may play a role in the development of this disease. Further research is required for a better understanding of the molecular and physiological mechanisms underlying the development of achalasia of the cardia.
- Hereditary factors: Some cases of achalasia may be linked to genetic factors that are inherited.
- Autoimmune disorders: Autoimmune processes in the body may contribute to the development of achalasia, where the immune system attacks its own tissues.
- Nerve imbalance: Various neurological disorders or damage to the nervous system can affect the functioning of the digestive system, including the cardiac sphincter.
- Degenerative changes: Gradual deterioration of the muscles and tissues of the esophagus over time may contribute to the development of achalasia.
- Other factors: Including possible viral infections, prolonged exposure to stress, or irritants to the esophagus.
Notable signs of Cardia Achalasia
Achalasia of the cardia is characterized by a variety of symptoms, including dysphagia (difficulty swallowing), regurgitation (return of food), chronic pressure in the chest, and pain when swallowing. Preceding diagnosis with specialized tests, patients with achalasia of the cardia may complain of a sensation of food getting stuck in their throat or chest. Progressive dysphagia, especially to semi-solid and liquid foods, is a characteristic symptom of achalasia of the cardia and can lead to a reduced nutritional status of the patient and a deterioration in their quality of life.
- Dysphagia: Difficulty swallowing is one of the main symptoms of cardia achalasia, especially when consuming solid and semi-solid foods.
- Regurgitation: Patients with cardia achalasia may feel food returning after eating, which can lead to disorientation and discomfort.
- Chest pressure: Chronic feelings of pressure or discomfort in the chest may be observed in patients with cardia achalasia, especially after meals.
- Pain when swallowing: Some patients with cardia achalasia may experience pain or discomfort when swallowing, which can affect their nutritional status and quality of life.
- Feeling of food blockage: Some individuals may complain of a sensation of food being stuck in the throat or chest, which becomes a problem in daily life and during meals.
The professionals’ perspective on the therapy of cardia achalasia
A significant number of experts in the treatment of cardiac achalasia recommend a combined approach that includes both conservative methods and surgical intervention. Pharmacological therapy aims to improve symptoms such as dysphagia and may include the use of vasodilators and botulinum therapy. However, surgical treatment, such as pneumodilation or myotomy, aims to restore normal cardiac function and is the preferred method when there is insufficient improvement from conservative therapy.
Moreover, experts acknowledge that an individualized approach to the treatment plan is a key element in the successful management of cardiac achalasia, considering various factors such as age, overall patient condition, and the stage of disease progression. Research continues to seek new treatment methods that could provide more effective symptom management and improve the quality of life for patients suffering from cardiac achalasia.

Checking and detecting Cardia Achalasia
Diagnosis of cardia achalasia is an important step preceding the designation of optimal treatment. To confirm the diagnosis, specialists typically use various methods, including esophagogastroduodenoscopy (EGDS) with biopsy, esophageal manometry to assess peristalsis and lower esophageal sphincter pressure, as well as esophagram with contrast. These methods help not only to confirm the presence of cardia achalasia but also to assess the severity of its manifestations, which is important for selecting the optimal treatment plan and further prognosis for the patient.
- Esophagogastroduodenoscopy (EGDS) with biopsy: This procedure allows for the visual examination of the esophagus, stomach, and duodenum by inserting a flexible endoscope through the patient’s mouth.
- Esophageal manometry: This study evaluates the muscle activity of the esophagus and the pressure of the lower esophageal sphincter during swallowing, aiding in the diagnosis of achalasia cardia.
- X-ray of the esophagus with contrast: The patient ingests a contrasting substance that makes the esophagus visible during X-ray imaging, helping to identify anomalies in the esophagus, including achalasia cardia.
- Diagnostic endoscopy: This procedure involves the endoscopist visually examining the esophagus and stomach using an endoscope, allowing for the detection of changes and pathologies in these organs.
- Computed tomography (CT) of the esophagus and stomach: This imaging method utilizing X-rays helps to detect anomalies and tumors in the area of the esophagus and stomach.
Principles of Therapy for Cardiac Achalasia
- Esophageal dilation: a procedure to widen the walls of the esophagus to improve passage.
- Botulinum therapy: a method involving the injection of botulinum toxin into the lower esophageal sphincter to induce relaxation.
- Surgical intervention: includes procedures such as myotomy and endoscopic methods aimed at eliminating the causes of cardia achalasia.
- Individual approach: it is important to consider the characteristics of each patient when choosing a treatment method for optimal results.
- Comprehensive therapy: treatment of cardia achalasia requires an integrated approach that combines various methods to achieve the best outcomes.
Measures to prevent achalasia of the cardia
- Proper nutrition: Regular consumption of healthy and balanced food contributes to the maintenance of digestive system health.
- Moderate physical activity: Physical activity helps maintain good function of the digestive system and overall body health.
- Avoiding overeating: Overeating can have negative consequences for digestion, so it is important to monitor portion sizes and not consume food in excess.
- Giving up bad habits: Smoking and alcohol consumption negatively impact the condition of the digestive organs, so their use should be minimized or completely eliminated.
- Timely consultation with a doctor: If symptoms that concern the patient appear, it is important to seek medical advice for the timely identification and treatment of possible pathologies, including cardia achalasia.