Alcoholic liver damage: signs, causes, and treatment methods
- Understanding Alcoholic Liver Damage: Explanation of Key Concepts
- Factors causing alcoholic liver damage
- Clinical picture of alcoholic liver damage
- Expert opinion on the methods of treating alcoholic liver damage
- Methods for diagnosing alcoholic liver damage
- Methods of treating alcoholic liver damage
- Measures for the prevention of alcoholic liver disease
- Interesting facts about alcoholic liver damage
- FAQ
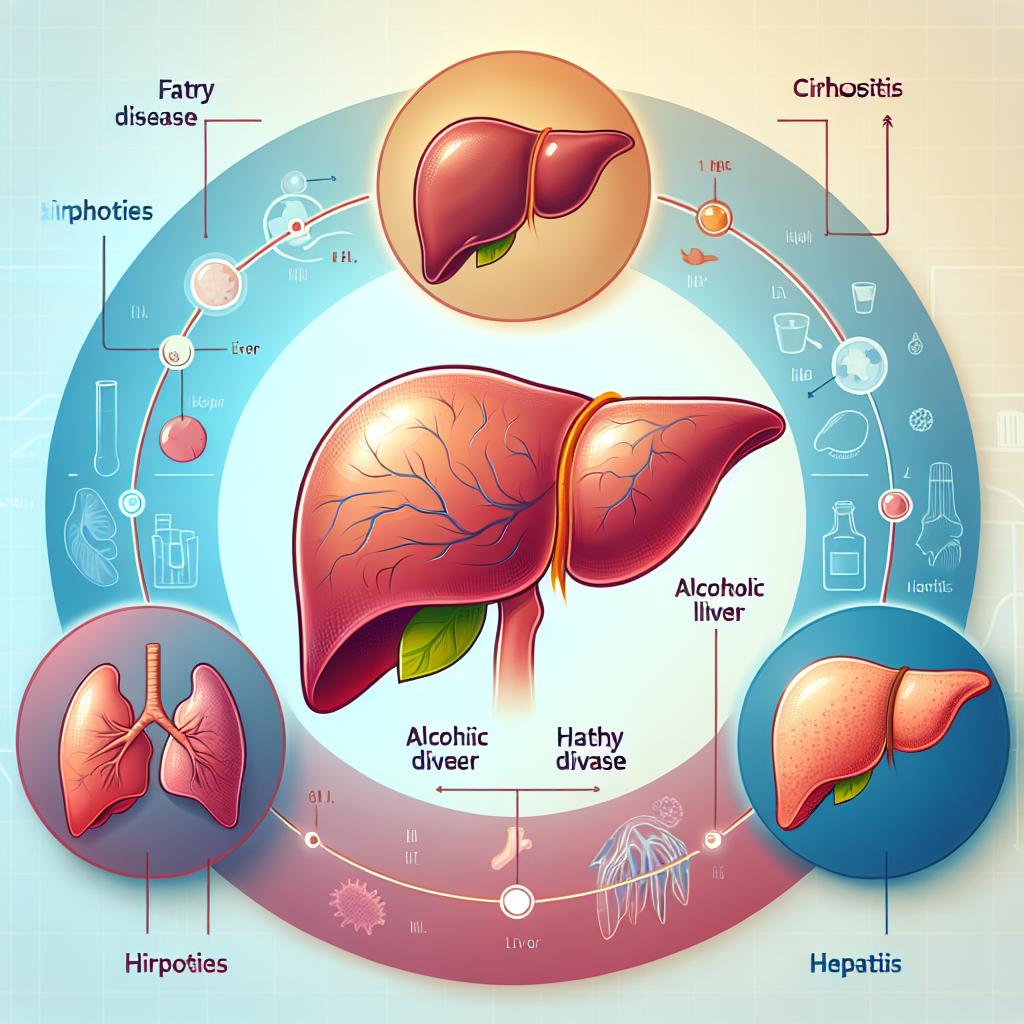
Understanding Alcoholic Liver Damage: Explanation of Key Concepts
Understanding alcoholic liver damage is an important aspect of medical practice. The main concepts related to this condition are the pathophysiology of liver failure development under the influence of alcohol, the mechanisms of fatty degeneration and inflammation in liver tissue, as well as the impact of alcohol on detoxification processes in the liver. Additionally, it is important to understand the role of genetic factors and the relationship between alcoholic liver damage and other diseases of the digestive organs. A deep knowledge of these key concepts allows for effective diagnosis and treatment of alcoholic liver damage, which is crucial for maintaining patient health.
Factors causing alcoholic liver damage
Alcoholic liver damage is caused by a complex of factors, including the direct toxic effect of ethanol and its metabolites on liver cells. Ethanol and acetaldehyde contribute to the development of inflammation, fatty degeneration, and liver fibrosis. Additionally, alcohol negatively impacts lipid and carbohydrate metabolism processes in the liver, leading to impaired liver function.
Prolonged and excessive alcohol consumption, especially combined with a diet high in fats, as well as genetic predisposition, can increase the risk of developing alcoholic liver damage. It is also important to note that individual sensitivity to alcohol and the presence of comorbid diseases can influence the progression of liver dysfunction with alcohol consumption.
- Direct toxic effect: Ethanol and its metabolites cause damage to the liver, leading to inflammation and fatty degeneration.
- Disruption of lipid and carbohydrate metabolism: Alcohol affects the processes of fat and carbohydrate metabolism in the liver, impairing its functions.
- Prolonged and excessive alcohol consumption: Frequent and excessive consumption of alcoholic beverages increases the risk of liver damage.
- Nutrition and lifestyle: The combination of alcohol with a diet rich in fats can enhance the impact on the liver.
- Genetic predisposition: The presence of certain genetic factors may increase the liver’s vulnerability to alcohol.
Clinical picture of alcoholic liver damage
The clinical picture of alcoholic liver disease may include a variety of symptoms and signs reflecting organ dysfunction. Patients often complain of fatigue, weakness, loss of appetite, nausea, discomfort in the abdominal area, and increased sensitivity to pain in the right upper quadrant. Among the typical symptoms of alcoholic liver disease, there may also be abdominal bloating, jaundice of the skin and sclera, the appearance of vascular “spider veins” on the skin, general weakness, and weight loss.
More severe conditions, such as liver cirrhosis, may manifest as ascites (accumulation of fluid in the abdominal cavity), portal hypertension, a vascular network on the abdomen, and disruption of blood flow and liver functions. A variant of alcoholic liver disease is alcoholic hepatitis, which is characterized by inflammation of the liver, jaundice, hepatomegaly, and may have an acute or chronic course depending on the degree of organ damage.
- Fatigue and weakness: One of the most common symptoms of alcoholic liver damage, associated with a general disruption of the organ’s functions.
- Loss of appetite: A decrease in the desire for food may be a result of liver dysfunction occurring due to alcoholic damage.
- Jaundice of the skin and sclera: A yellowish tint to the skin and the whites of the eyes may indicate impaired liver function and a high level of bilirubin in the blood.
- Abdominal bloating: Accumulation of fluid in the abdominal cavity, caused by liver damage, can lead to an increase in abdominal size.
- Skin “spider veins”: The appearance of “spiderwebs” of small vessels on the skin may be a sign of liver damage and impaired circulation.
Expert opinion on the methods of treating alcoholic liver damage
Experts in the fields of gastroenterology and hepatology express a unanimous opinion on the importance of a comprehensive approach to the treatment of alcohol-related liver damage. The main treatment methods include cessation of alcohol consumption, dietary therapy, medication, and, in some cases, surgical intervention. First and foremost, it is essential to focus on stopping alcohol consumption, as this is the primary factor causing liver damage.
Experts recommend using medications to support the liver, restore its functions, and reduce inflammation. Additionally, dietary therapy plays a crucial role in the treatment process of alcohol-related liver damage. Specialists also emphasize the necessity of regular monitoring of the patient’s condition, conducting dynamic examinations, and maintaining regular control of liver functions for effective treatment and prevention of complications.

Methods for diagnosing alcoholic liver damage
The diagnosis of alcoholic liver damage involves a comprehensive approach based on clinical manifestations, laboratory tests, and instrumental studies. Doctors may use data from the medical history, physical examinations, and patient complaints in conjunction with the results of biochemical blood tests, including levels of liver enzymes, bilirubin, proteins, and other markers of liver damage. To confirm the diagnosis and assess the severity of liver damage, instrumental studies are often conducted, including ultrasound, computed tomography, magnetic resonance imaging, and liver biopsy.
Particular attention is paid to assessing the degree of fibrosis (fibroscan) to evaluate the extent of fibrosis and cirrhosis of the liver. Diagnostic methods for alcoholic liver damage not only help establish the diagnosis but also determine the treatment strategy, prognosis, and possible complications in this condition.
- Biochemical blood tests: Examination of levels of liver enzymes, bilirubin, aminotransferases, and other markers of liver function.
- Ultrasound examination: Use of sound waves to visualize the structure and condition of the liver, determining its size and degree of changes.
- Computed tomography (CT): X-ray examination to obtain detailed images of the liver using a computer and X-ray radiation.
- Magnetic resonance imaging (MRI): Innovative liver visualization method using magnetic fields and radio waves that provides high detail.
- Liver elastography (fibroscan): Use of a special device to assess the degree of fibrosis and cirrhosis of the liver without the need for a biopsy.
Methods of treating alcoholic liver damage
In addition to medication therapy, an important component of treatment is dietary therapy. Specialists recommend following a diet rich in nutrients and proteins, as well as limiting the intake of fats and sugars. Regular physical exercise can also contribute to improving metabolism and the overall condition of the liver. In more severe cases, when complications are present, surgical intervention may be required, such as liver transplantation, especially in cases of cirrhosis or other irreversible changes in the organ.
- Ceasing alcohol consumption: The main and most important step in the treatment of alcoholic liver damage, contributing to the reduction of further injuries and the restoration of the organ’s tissues.
- Medication therapy: The use of specific drugs, such as detoxification agents, antioxidants, anti-inflammatory medications, and vitamins, aimed at improving liver function and reducing inflammation.
- Diet therapy: Following a diet rich in nutrients and proteins, limiting fats and sugars, promoting regeneration and recovery of the liver.
- Physical exercise: Regular physical activity can improve metabolism, reduce excess weight, and contribute to overall liver health.
- Surgical intervention: In cases of complications, such as cirrhosis or irreversible changes, a liver transplant may be required to save the patient’s life and restore the organ’s functions.
Measures for the prevention of alcoholic liver disease
An important aspect of preventing alcohol-related liver damage is also adhering to a healthy lifestyle, which includes regular physical exercise, balanced nutrition, quitting smoking, and avoiding drug use. Maintaining a healthy weight, regular medical check-ups to monitor liver health, and timely consultation with a doctor at the first signs of symptoms will help prevent the onset of alcohol-related liver damage and keep the organ in optimal condition.
- Refusal of excessive alcohol consumption: Complete and timely cessation of alcohol intake will help prevent the development of liver damage and maintain its health.
- Adherence to a healthy lifestyle: Regular physical exercise, healthy eating, and avoiding harmful habits such as smoking and drug use contribute to the overall health of the body, including the liver.
- Maintaining a healthy weight: Avoiding excess weight and obesity reduces the risk of developing fatty liver disease and other pathologies.
- Regular medical check-ups: Conducting periodic examinations to monitor liver condition allows for early detection of possible changes in the organ and timely intervention.
- Consulting a doctor upon the appearance of symptoms: Prompt response to the first signs of liver failure, such as fatigue, abdominal discomfort, and loss of appetite, will help initiate treatment in a timely manner and prevent the development of complications.
Interesting facts about alcoholic liver damage
Moreover, alcoholic liver damage can have not only physical but also psychological consequences. People suffering from liver pathologies often experience emotional and mental negative impacts, as they may feel shame or guilt due to their lifestyle or anxiety about the prognosis of their condition. Psychological support and understanding of this aspect can play an important role in the treatment and rehabilitation of patients with alcoholic liver damage.