Allergic rhinitis: symptoms, causes, and treatment
- Definition of allergic rhinitis
- Often, rhinitis is caused by allergies.
- The main signs of allergic rhinitis
- Effective methods for treating allergic rhinitis
- Methods for diagnosing allergic rhinitis
- Effective methods for treating allergic rhinitis
- Preventive measures for allergic rhinitis
- Interesting aspects of allergic rhinitis
- FAQ
Definition of allergic rhinitis
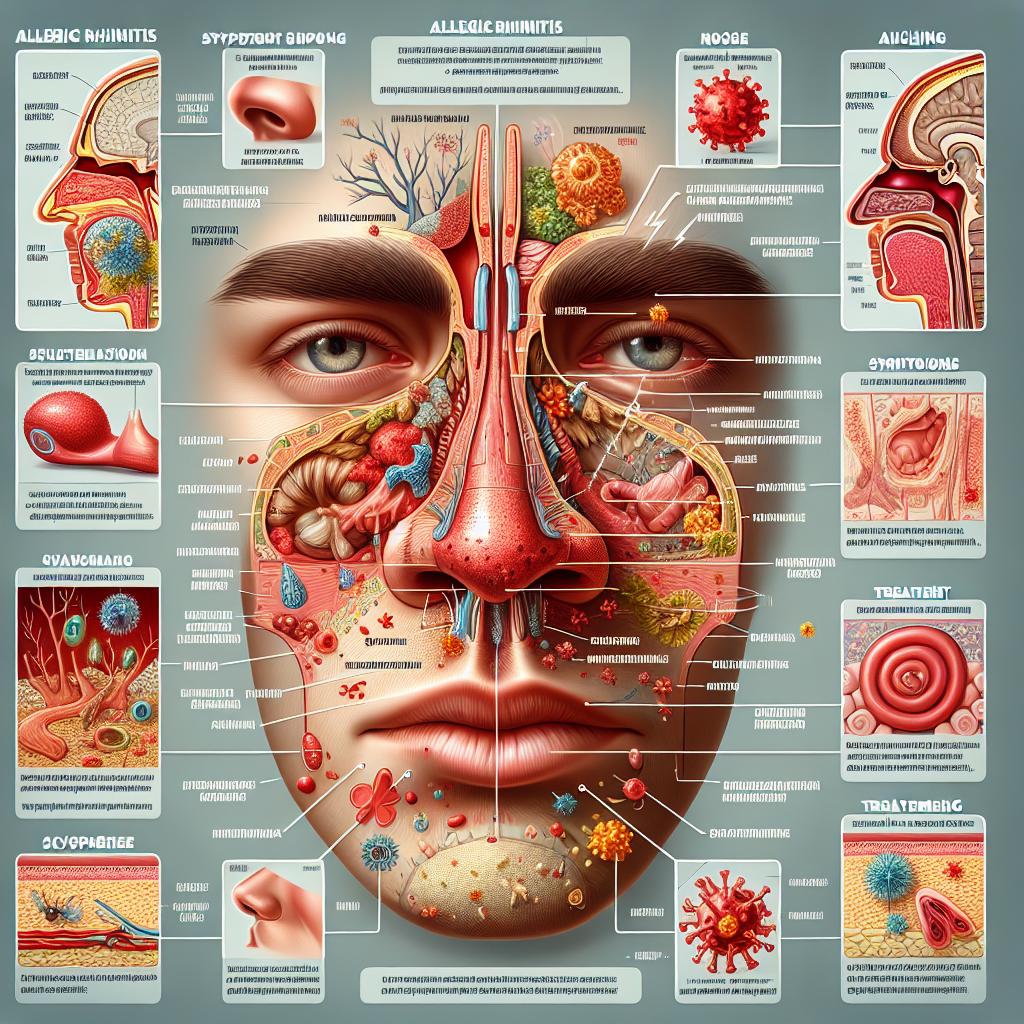
Allergic rhinitis is an inflammatory disease of the nasal mucosa caused by an allergic reaction to certain airborne allergens. This condition is characterized by various symptoms such as runny nose, nasal congestion, sneezing, and itching in the nose, which can significantly impair the patient’s quality of life.
The definition of allergic rhinitis includes identifying the allergic nature of the symptoms, conducting allergy tests, and examining the nasal cavity. Treatment of allergic rhinitis involves identifying the allergen and avoiding contact with it, using antihistamines, inhaled corticosteroids, and in some cases, immunotherapy.
Often, rhinitis is caused by allergies.
Allergic rhinitis, often referred to as “hay fever,” is a reaction of the body to allergens such as pollen, dust, fluff, mold, or animal dander. Upon contact with these allergens, the immune system begins to produce antibodies, leading to the release of substances that cause inflammation in the nasal sinuses.
It is important to note that the presence of a genetic predisposition to allergic reactions, as well as environmental influences and everyday toxins, can contribute to the onset of allergic rhinitis. Prolonged exposure to allergens and poor hygiene may also exacerbate the symptoms of rhinitis, making it one of the most common types of chronic upper respiratory diseases.
- Environmental allergens: pollen, dust, fluff, mold, and animal dander can cause allergic rhinitis.
- Genetic predisposition: a family history of allergic diseases can increase the likelihood of developing allergic rhinitis.
- Environmental exposure: prolonged contact with polluted air, tobacco smoke, and other toxins can contribute to the development of rhinitis symptoms.
- Insufficient hygiene: lack of cleanliness in the environment, infrequent changing of bed linen, or insufficient cleaning of surfaces can also worsen allergic rhinitis.
- Prolonged contact with allergens: daily work or living in areas with high levels of allergens can lead to chronic allergic rhinitis.
The main signs of allergic rhinitis
Allergic rhinitis manifests with a variety of symptoms, including runny nose, nasal congestion, sneezing, itching in the nose and eyes. Patients may also experience tearing, coughing, decreased sense of smell, and fatigue. Symptoms typically worsen upon contact with allergens and can significantly reduce the quality of life for patients.
For an accurate diagnosis of allergic rhinitis, it is important to pay attention to the nature and duration of symptoms, as well as the presence of factors that exacerbate the condition. A medical examination, including an inspection of the nasal cavity and allergy tests, will help confirm the diagnosis and determine the most effective treatment for each specific case.
- Runny nose: is characterized by excessive secretion of mucus from the nose, which can be either clear or thick, and can also lead to a feeling of mucus accumulation in the nose.
- nasal congestion: arises from swelling of the nasal mucous membranes and may be accompanied by difficulty breathing and a sensation of fullness in the nose.
- Sneezing: a reflex response to irritation of the nasal mucous membrane, combined with a quick and forceful exhalation aimed at clearing the airways.
- Itching in the nose and eyes: the sensation of itching and discomfort in the area of the nose and eyes may be one of the first signs of allergic rhinitis.
- Watery eyes: increased tear secretion in allergic rhinitis is caused by irritation of the eye mucous membranes by allergens.
Effective methods for treating allergic rhinitis
Experts in the field of allergology recommend a comprehensive approach to treating allergic rhinitis, which includes identifying the allergen, avoiding contact with it, using antihistamines, and inhaled corticosteroids. These methods help reduce inflammation of the nasal mucosa, alleviate symptoms, and improve the quality of life for patients with this condition.
Additionally, some experts also emphasize the importance of immunotherapy in the treatment of allergic rhinitis, especially in cases where other treatment methods prove to be insufficiently effective. Immunotherapy allows for increased tolerance to the allergen, reducing the body’s sensitivity and improving the overall condition of patients with allergic rhinitis.

Methods for diagnosing allergic rhinitis
Diagnosis of allergic rhinitis includes studying the medical history, examining the nasal cavity for edema and changes in the mucous membrane, as well as conducting allergy tests to identify specific allergens that trigger the reaction. Clarifying detailed symptoms and performing a physical examination allows the doctor to establish a diagnosis of allergic rhinitis and determine the optimal treatment course.
Additional diagnostic methods, such as rhinofibroscopy, computed tomography of the nasal cavity, and analysis of mucus for inflammatory markers, may be used for accurate identification of the degree of inflammation and complications in the nasal cavity of patients with allergic rhinitis. Effective diagnosis allows for individualized treatment and ensures optimal disease control.
- Symptom analysis: the doctor conducts a detailed study of the nature of the patient’s symptoms, including a runny nose, nasal congestion, sneezing, itching, and other manifestations of airway disturbances.
- Physical examination: the doctor may examine the patient’s nasal cavity for swelling, redness of the mucous membrane, and other characteristic signs of allergic rhinitis.
- Allergy tests: conducting skin allergy tests or immunological analyses can help identify specific allergens that trigger reactions in the patient’s body.
- Rhinofibroscopy: a method of examining the nasal cavity using a special instrument, allowing assessment of the mucous membrane’s condition and detection of possible changes.
- Computed tomography of the nasal cavity: the use of CT allows detailed images of the nasal sinuses to be obtained and structural changes associated with allergic rhinitis to be assessed.
Effective methods for treating allergic rhinitis
For long-term control of allergic rhinitis, immunotherapy may be considered an effective method. Immunotherapy helps improve tolerance to the allergen, reducing sensitivity to it and decreasing reactions to allergens. It is important to consult qualified specialists to determine the optimal treatment plan, taking into account the individual characteristics of each patient and the severity of the disease’s manifestations.
- Antiallergenic drugs: antihistamines and inhaled glucocorticoids can reduce inflammation and alleviate symptoms of allergic rhinitis.
- Decongestants: the use of decongestants helps combat nasal congestion and mucosal swelling, easing breathing and reducing discomfort.
- Immunotherapy: this treatment method aims to improve tolerance to allergens and reduce the body’s sensitivity to them, which can significantly lessen reactions to allergens.
- Avoidance of contact with allergens: preventing contact with known allergens, such as pollen or dust, can help reduce symptoms of allergic rhinitis.
- Non-medical methods: include using wet wipes, regular cleaning of the premises, using hypoallergenic bedding, and other measures to reduce contact with potential allergens.
Preventive measures for allergic rhinitis
A significant aspect of preventing allergic rhinitis is the timely identification of allergic reactions and promptly consulting a doctor for recommendations and treatment. Educating patients on symptom management methods, proper use of medications, and implementing lifestyle change recommendations can play an important role in preventing the development and reducing the manifestations of allergic rhinitis.
- Adherence to a hypoallergenic diet: excluding food products that may be allergens helps reduce the risk of developing allergic rhinitis.
- Regular cleaning of the premises: maintaining cleanliness in the space reduces the concentration of dust, mold, and other potential allergens, thereby aiding in the prevention of rhinitis.
- Avoiding contact with pets: for individuals suffering from allergic rhinitis, it is important to limit contact with animals, as fur, skin secretions, and saliva can trigger an allergic reaction.
- Maintaining optimal humidity levels: using humidifiers in the room can reduce dryness in the mucous membranes and decrease the risk of developing rhinitis.
- Monitoring environmental conditions: avoiding areas with high levels of pollen, mold, and other allergens helps prevent the onset of allergic rhinitis symptoms.
Interesting aspects of allergic rhinitis
It is also interesting that the symptoms of allergic rhinitis can mimic a cold or upper respiratory infection, which can complicate the correct diagnosis. Patients suffering from allergic rhinitis may experience a significant decrease in quality of life due to constant discomfort. In this regard, it is important to conduct differential diagnosis and develop an individualized treatment plan for each patient.