Amenorrhea: diagnosis, classification, and treatment methods
Clarification of the concept of amenorrhea
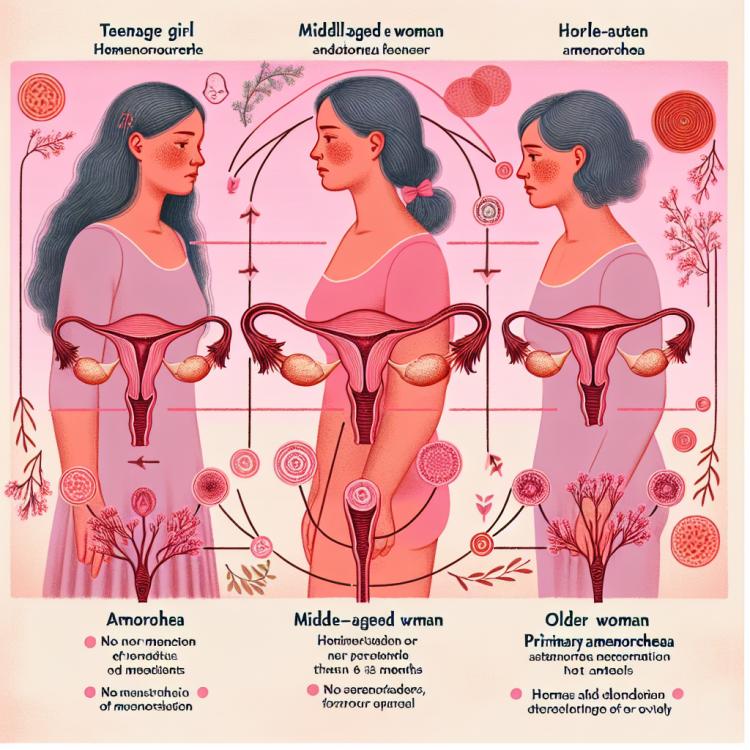
Amenorrhea is a condition in which a woman experiences the absence of menstruation for a certain period of time. This can result from various physiological anomalies, including hormonal disorders, developmental abnormalities of the reproductive system, possible endocrine disorders, or even psychological factors. The diagnosis of amenorrhea requires a comprehensive approach, including medical history, physical examination, laboratory, and instrumental studies to identify the underlying cause of the absence of menstruation in a specific patient.
Possible causes of amenorrhea
The causes of amenorrhea can be diverse and include various pathological conditions. One common factor is hypothalamic amenorrhea, caused by an imbalance in the hypothalamic-pituitary-ovarian system due to stress, malnutrition, intense physical exertion, or other external influences. Other causes may include hormonal disorders, ovarian cysts, polycystic ovarian syndrome, hyperprolactinemia, hypothyroidism, or other endocrine disorders, as well as developmental abnormalities of the reproductive system. Additionally, psychological stress, eating disorders, obesity, or weight irregularities can also contribute to the development of amenorrhea.
- Hypothalamic amenorrhea: occurs due to an imbalance in the hypothalamus, most often caused by stress or malnutrition.
- Hormonal disorders: changes in hormone levels, such as prolactin, estrogens, or progesterone, can lead to amenorrhea.
- Polycystic ovary syndrome: a condition in which multiple cysts develop on the ovaries, causing hormonal imbalance.
- Endocrine disorders: such as hypothyroidism or hyperprolactinemia can be the cause of amenorrhea.
- Psychological stress: emotional strain and psychological problems can disrupt the menstrual cycle and lead to amenorrhea.
Main signs of amenorrhea
The main signs of amenorrhea can be diverse and individually depend on the underlying cause of this condition. The absence of menstruation for more than six months in women of reproductive age can be considered one of the key symptoms of amenorrhea. Menstrual cycle disorders, changes in the length and regularity of the cycle, as well as various accompanying symptoms, such as changes in weight, headaches, sleep disturbances, and increased fatigue, may also indicate a possible presence of amenorrhea and require further medical examination and diagnosis.
- Absence of menstruation: One of the main symptoms of amenorrhea is the absence of menstruation for six months in women of reproductive age.
- Menstrual cycle disorders: Changes in cycle length, irregularity, or complete absence of the cycle may indicate disruptions in the reproductive system’s function.
- Weight changes: Unexplained weight loss or gain may be associated with amenorrhea, as weight and nutrition play an important role in the functioning of the menstrual cycle.
- Headaches: Many women with amenorrhea may experience headaches and migraines, which can be linked to hormonal imbalance and physiological changes.
- Fatigue and sleep disturbances: Frequent feelings of tiredness, increased drowsiness, and sleep disturbances may accompany amenorrhea due to changes in the body and emotional stress.
Experts’ views on the treatment of amenorrhea
Experts in the fields of gynecology and reproductive health emphasize the importance of a personalized approach to the treatment of amenorrhea. Identifying the root cause of the absence of menstruation in each woman is a key step in developing an optimal treatment strategy. This may include medication therapy to restore hormonal balance, dietary adjustments, psychotherapeutic support in cases of psychogenic factors, as well as physical rehabilitation in cases where amenorrhea is caused by intense physical exertion or pathologies of the reproductive system.
In cases where underlying health conditions such as polycystic ovary syndrome (PCOS), thyroid disorders, or pituitary abnormalities are identified as the cause of amenorrhea, experts suggest targeted treatment aimed at addressing the specific medical issue. Surgical intervention may be necessary in certain cases, such as the removal of ovarian cysts or correction of structural abnormalities. Monitoring and follow-up care are essential components of the treatment plan to ensure the effectiveness of interventions and to address any potential complications or recurrences.

Methods for diagnosing amenorrhea
Diagnosis of amenorrhea involves a comprehensive investigation aimed at identifying the underlying cause of the absence of menstruation. The doctor may conduct a detailed examination of the patient, including medical history, physical examination, and laboratory tests to assess the hormonal status. Instrumental diagnostic methods, such as ultrasound of the pelvic organs or magnetic resonance imaging, may be prescribed to evaluate the condition of the reproductive system and identify possible changes in the ovaries, uterus, or pituitary gland that may be associated with the development of amenorrhea.
Additional diagnostic methods may include blood tests to determine hormone levels such as prolactin, estrogens, progesterone, gonadotropic hormones, and thyrotropin, as well as functional tests to clarify the diagnosis and determine the treatment strategy appropriate for the specific case.
- Medical history: The doctor collects information about the menstrual cycle, previous health changes, the presence of stressful situations, weight changes, and other factors that may be related to the development of amenorrhea.
- Physical examination: The doctor conducts an examination of the patient to identify physical anomalies or signs that may indicate the causes of amenorrhea, such as hypothyroidism, polycystic ovary syndrome, or hyperprolactinemia.
- Laboratory tests: Include blood tests to determine hormone levels such as prolactin, estrogens, progesterone, gonadotropic hormones, and thyrotropin, as well as other biochemical parameters.
- Ultrasound examination of the pelvic organs: Allows visualizing the condition of the ovaries, uterus, and other organs to identify possible anomalies or pathologies contributing to the development of amenorrhea.
- Magnetic resonance imaging (MRI): May be used for a more detailed assessment of the hypothalamus, pituitary gland, and other structures if there is suspicion of hypothalamic amenorrhea or other central nervous system issues.
Methods of treating amenorrhea
In some cases, especially with anomalies in the structure of the reproductive system or pituitary tumors, surgical intervention may be required. For example, the removal of ovarian cysts or the correction of pituitary pathologies may allow for the restoration of normal ovarian function and hormonal balance. Effective treatment of amenorrhea requires an individual approach and comprehensive investigation to determine the optimal strategy in each specific clinical case.
- Hormonal therapy: Involves the use of medications containing female sex hormones (estrogens, progesterone) to restore hormonal balance and stimulate menstrual function.
- Psychotherapy: For women with amenorrhea caused by stress or other psychological factors, consultations with specialists in psychosomatics may help restore menstrual function.
- Surgical intervention: In cases requiring correction of abnormalities in the reproductive system or pituitary tumors, surgery may be necessary to restore normal organ function and hormonal balance.
- Diet therapy: Rational nutrition and weight control may be important components of treating amenorrhea, especially when weight or dietary disturbances are risk factors.
- Therapy for restoring psycho-emotional state: Includes methods of psychological support, relaxation, and stress resilience to improve mental well-being and normalize the menstrual cycle.
Measures for the prevention of amenorrhea
Regular consultations with a gynecologist and conducting tests to monitor hormone levels and the state of the reproductive system will also help detect early signs of menstrual cycle disorders and take timely preventive measures against amenorrhea. Education about a healthy lifestyle, including understanding the impact of nutrition, physical activity, and psycho-emotional well-being on reproductive health, also plays an important role in preventing potential menstrual function disorders.
- Maintaining a healthy weight: Maintaining normal weight and avoiding extreme diets and nutritional imbalances contribute to preserving a normal menstrual cycle.
- Regular physical activity: Moderate physical exercise promotes overall health and positively impacts reproductive health, helping to prevent potential cycle disorders.
- Healthy eating: A balanced and varied diet enriched with vitamins and minerals plays an important role in maintaining hormonal balance and the functioning of the reproductive system.
- Regular visits to the doctor: Regular consultations with a gynecologist and tests to monitor hormone levels and the state of the reproductive system will help identify problems at early stages and prevent the development of amenorrhea.
- Education on a healthy lifestyle: Conducting informational campaigns, including those on healthy eating, physical activity, stress resilience, and the impact of these factors on reproductive health, contributes to the prevention of amenorrhea and other menstrual function disorders.
Interesting features of amenorrhea
Another interesting fact is that amenorrhea can be a marker for certain diseases, such as polycystic ovary syndrome (PCOS), hypothyroidism, hyperprolactinemia, or even pituitary tumors. Therefore, when amenorrhea occurs, it is important to conduct a comprehensive examination to identify the underlying cause, which may require individualized treatment. Studies and observations show that timely diagnosis and a careful approach to treating amenorrhea contribute to the restoration of a normal menstrual cycle and the maintenance of reproductive health.