Amyloidosis of the kidneys: everything you need to know
- Understanding kidney amyloidosis
- Factors contributing to the development of kidney amyloidosis
- Main manifestations of kidney amyloidosis
- Approaches to the treatment of renal amyloidosis: experts’ opinions
- Methods for diagnosing kidney amyloidosis
- Methods of treating kidney amyloidosis
- Prevention measures for kidney amyloidosis
- Amazing features of kidney amyloidosis
- FAQ
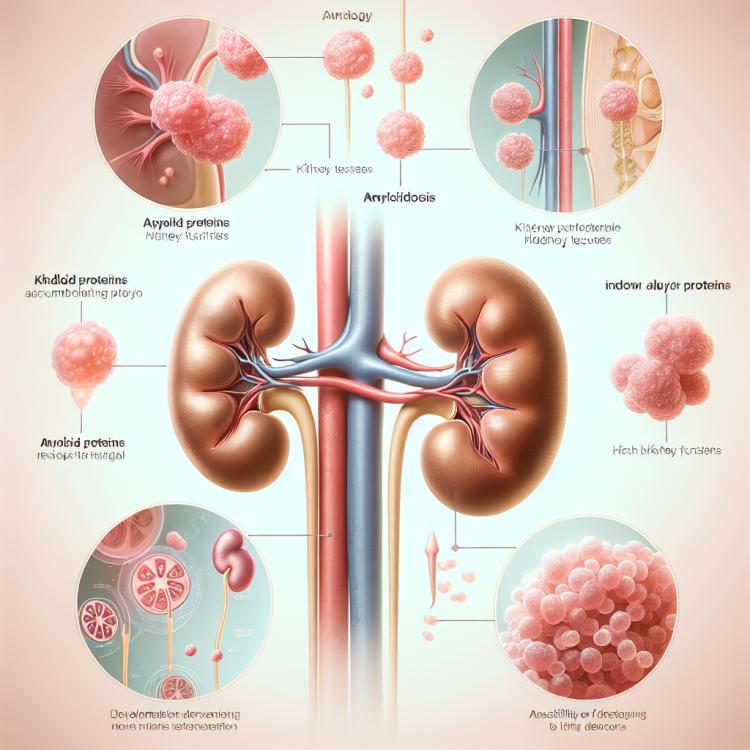
Understanding kidney amyloidosis
Amyloidosis of the kidneys is a rare disease characterized by the deposition of amyloid in the kidney tissue. Amyloid is an insoluble protein that can accumulate in various organs, causing disorders and dysfunctions.
As kidney amyloidosis develops, there is a gradual deterioration in kidney function, which can lead to chronic kidney failure. Patients with kidney amyloidosis may experience symptoms such as protein in the urine, swelling, and increased blood pressure.
Factors contributing to the development of kidney amyloidosis
Factors that contribute to the development of kidney amyloidosis may include hereditary predispositions, prolonged chronic inflammation, tumors, as well as certain disorders of protein metabolism in the body. For example, patients with multiple myeloma often experience the deposition of amyloid protein in the kidneys, which can lead to the development of amyloidosis.
In addition, systemic diseases such as rheumatoid arthritis and systemic lupus erythematosus, as well as chronic infectious processes, may provoke the development of kidney amyloidosis. It is important to know and consider these factors in the diagnosis and treatment of patients suspected of having kidney amyloidosis.
- Hereditary factors: Genetic mutations may contribute to the tendency to develop amyloidosis of the kidneys.
- Chronic inflammation: Continuous inflammatory processes in the body can stimulate the formation of amyloid in the kidneys.
- tumors: Certain types of tumors may be associated with the onset of kidney amyloidosis.
- Protein metabolism disorders: Various disorders in protein metabolism can lead to the deposition of amyloid in kidney tissues.
- Autoimmune diseases: Systemic diseases of the immune system may be one of the factors in the development of kidney amyloidosis.
Main manifestations of kidney amyloidosis
The main manifestations of kidney amyloidosis are proteinuria, which is the presence of protein in the urine, edema, and a gradual decline in kidney function. Protein in the urine can be one of the first signs of the disease, as amyloid damages the kidney glomeruli, leading to the leakage of protein into the urine. Edema, especially in the areas of the face, hands, and legs, may also be noted as a consequence of declining kidney function and fluid retention in the body.
As kidney function deteriorates, symptoms of kidney failure may appear, such as high blood pressure, fatigue, anemia, itchy skin, changes in appetite, and sleep disturbances. Early detection and treatment of kidney amyloidosis are important to prevent the progression of the disease and preserve kidney function in patients.
- Proteinuria: The presence of protein in the urine is one of the main symptoms of kidney amyloidosis, resulting from damage to the kidney glomeruli by amyloid.
- Edema: Gradual accumulation of fluid in the body leads to edema, which often manifests in the areas of the face, limbs, and abdomen.
- Worsening kidney function: As kidney amyloidosis progresses, kidney function deteriorates, which can manifest as high blood pressure, fatigue, anemia, and other signs of kidney failure.
- Increased pressure: One of the symptoms of kidney amyloidosis may be elevated blood pressure, caused by disturbances in the fluid and electrolyte balance regulation system.
- Changes in urination: Patients with kidney amyloidosis may experience changes in the frequency and volume of urination, which may also be one of the signs of the disease.
Approaches to the treatment of renal amyloidosis: experts’ opinions
Experts in nephrology and rheumatology agree that the treatment of kidney amyloidosis should be comprehensive and aimed at controlling the symptoms of the disease, improving kidney function, and slowing disease progression. The main approaches include treating the underlying disease that contributes to the development of amyloidosis, such as rheumatoid arthritis or multiple myeloma, as well as symptomatic therapy to reduce proteinuria, control blood pressure, and improve kidney function.
Optimal management of kidney amyloidosis requires an individualized approach that takes into account the unique aspects of each clinical case. Experts also emphasize the need for continuous monitoring of the patient’s condition, laboratory indicators of kidney function, and the effectiveness of ongoing therapy to achieve the best outcomes in the treatment of kidney amyloidosis.

Methods for diagnosing kidney amyloidosis
Diagnosis of kidney amyloidosis is a multifaceted process aimed at identifying the signs and symptoms of the disease. A key diagnostic method is kidney tissue biopsy, which allows for the detection of amyloid deposits under a microscope. Additional examination methods may include urine tests for protein and other indicators, imaging of the kidneys using ultrasound or computed tomography, as well as biochemical and immunological tests.
In the early stages, kidney amyloidosis can be challenging to diagnose due to often negative results from standard tests, making it important to strive for a comprehensive diagnostic approach involving experienced specialists. Based on a comprehensive clinical picture and the results of examinations, doctors can make an accurate diagnosis and choose the optimal treatment plan for patients with kidney amyloidosis.
- Kidney tissue biopsy: A key diagnostic method that allows determining the presence of amyloid deposits under the microscope and confirming the diagnosis of kidney amyloidosis.
- Urine analysis: Evaluation of urine for protein and other indicators helps identify possible changes and damage to the kidneys characteristic of amyloidosis.
- Imaging of the kidneys: Ultrasound, computed tomography, or magnetic resonance imaging helps visualize kidney changes characteristic of amyloidosis.
- Biochemical tests: Blood tests for the levels of amyloid protein, creatinine, and other chemical indicators are used to assess kidney function and disease dynamics.
- Immunological tests: Additional studies for antibodies and inflammation markers may help clarify the diagnosis of kidney amyloidosis and determine possible causes of the disease.
Methods of treating kidney amyloidosis
Additionally, patients with kidney amyloidosis may be prescribed symptomatic therapy to improve quality of life and reduce manifestations of the disease, such as swelling, elevated blood pressure, and fatigue. The optimal treatment plan is developed taking into account the individual characteristics of each patient and requires a comprehensive approach based on modern standards of medical practice.
- Treatment of the underlying disease: The main strategy in the treatment of kidney amyloidosis is to address the underlying disease that triggered the deposition of amyloid, such as rheumatoid arthritis, multiple myeloma, or other systemic diseases, in order to reduce the burden on the kidneys.
- Blood pressure control: Maintaining normal blood pressure levels is an important component of kidney amyloidosis treatment, as high blood pressure can worsen kidney function and promote disease progression.
- Regulation of protein metabolism: Correcting protein metabolism disorders to reduce amyloid deposition in tissues and kidneys is one of the treatment strategies for amyloidosis.
- Reduction of proteinuria: Decreasing protein excretion in urine through pharmacological therapy can help reduce kidney damage and slow disease progression.
- Symptomatic therapy: Treatment of symptoms such as edema, high blood pressure, and other manifestations of kidney amyloidosis aims to improve the quality of life for patients and reduce the negative impact of the disease on the body.
Prevention measures for kidney amyloidosis
Regular medical examinations and monitoring of kidney condition can also contribute to the early detection of primary signs of kidney pathology, including amyloidosis. Implementing preventive measures under the supervision of specialists will allow for timely adjustments to diet, necessary medication, and the maintenance of kidney health to prevent the progression of amyloidosis and preserve kidney function.
- Control of underlying diseases: The basis for the prevention of kidney amyloidosis is timely and effective treatment of underlying diseases, such as rheumatoid arthritis or systemic inflammatory processes, to prevent the development of amyloid deposits in the kidneys.
- Healthy lifestyle: Maintaining a healthy lifestyle, including moderate physical activity, a balanced diet with reduced salt and fat intake, avoiding smoking, and moderate alcohol consumption, contributes to overall health and reduces the risk of diseases that can lead to kidney amyloidosis.
- Regular medical check-ups: Conducting regular medical examinations, including blood and urine tests, measuring blood pressure, and assessing kidney function, helps to detect changes and risks of developing kidney diseases, including amyloidosis, at an early stage.
- Specialist assistance: Under the consultation of nephrologists and rheumatologists, an individual prevention plan is developed that may include recommendations on diet, medication intake, and maintaining overall health.
- Educational programs: Participating in educational programs and events on the prevention of kidney diseases provides up-to-date information on ways to protect the kidneys and take measures to prevent amyloidosis.
Amazing features of kidney amyloidosis
Another surprising aspect is the difficulty in diagnosing kidney amyloidosis, as the disease can mimic other kidney pathologies. Identifying amyloidosis requires a comprehensive approach, including a kidney tissue biopsy and laboratory tests. Despite the rarity of the disease, timely diagnosis and effective treatment are crucial for preserving kidney function and the overall health of the patient.