Antiphospholipid syndrome: symptoms, causes, and treatment
- Understanding antiphospholipid syndrome
- Factors contributing to the development of antiphospholipid syndrome
- Clinical manifestations of antiphospholipid syndrome
- Approaches to the treatment of antiphospholipid syndrome recommended by experts
- Methods for diagnosing antiphospholipid syndrome
- Strategies for treating antiphospholipid syndrome
- Strategies for the prevention of antiphospholipid syndrome
- Amazing features of antiphospholipid syndrome
- FAQ
Understanding antiphospholipid syndrome
Antiphospholipid syndrome (APS) is an autoimmune disease characterized by elevated levels of antibodies to phospholipids, which can lead to thromboses and placental damage in pregnant women. The main manifestations of APS include recurrent thromboses and an increased risk of complications during pregnancy, such as premature birth and stillbirth. The mechanisms of disease development are related to hemostasis disorders and inflammation, leading to thrombosis formation and vascular damage, which requires a comprehensive approach to diagnosis and treatment.
Factors contributing to the development of antiphospholipid syndrome
The development of antiphospholipid syndrome (APS) may be influenced by various factors, including genetic predisposition, autoimmune disorders, and environmental exposure. The presence of certain genetic mutations, such as the Factor V Leiden mutation or the prothrombin mutation, may contribute to an increased risk of thrombosis and, consequently, the development of APS. Autoimmune factors, such as the presence of antibodies to phospholipids, may also play an important role in the pathogenesis of this syndrome, causing disruptions in the coagulation and inflammation systems, leading to thrombosis and other clinical manifestations of APS.
- Autoimmune disorders: The presence of antibodies to phospholipids can cause dysregulation of the immune system, contributing to the development of antiphospholipid syndrome.
- Genetic predisposition: The presence of certain genetic mutations, such as factor V Leiden mutation or prothrombin mutation, can increase the risk of thrombosis and APS.
- Inflammatory processes: Chronic inflammatory conditions can contribute to an imbalance in the coagulation system and inflammation of the vessels, promoting the development of the syndrome.
- Use of certain medications: Some medications, such as hormonal agents or certain antibiotics, may promote the development of antiphospholipid syndrome.
- Environmental exposure: Environmental factors, such as smoking or stress, can increase the risk of developing APS by negatively impacting the coagulation system and the immune system.
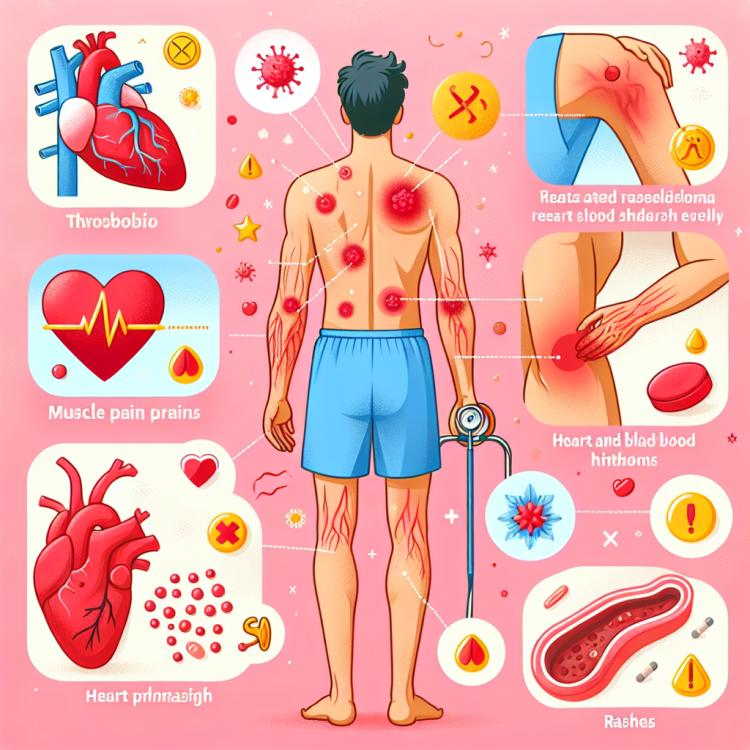
Clinical manifestations of antiphospholipid syndrome
The clinical manifestations of antiphospholipid syndrome (APS) vary from case to case, however, the main symptoms include recurrent thromboses, especially venous thromboses, such as deep vein thromboses or pulmonary artery thromboses. Patients with APS also often exhibit elevated levels of antibodies to phospholipids, which is one of the diagnostic criteria for this syndrome. In women, APS can lead to an increased risk of pregnancy complications, including premature birth, miscarriage, and preeclampsia, which requires special attention when managing pregnant patients with APS.
- Recurrent thrombosis: Patients with antiphospholipid syndrome often face repeated cases of thrombosis, especially in the venous system, which can lead to serious complications such as pulmonary embolism.
- Elevated antibodies to phospholipids: A diagnostic criterion for APS is the presence of antibodies to phospholipids in the patient’s blood, which may be associated with the occurrence of thrombotic events and other pathological processes.
- Pregnancy complications: Women with APS have an increased risk of complications during pregnancy, including premature birth, miscarriage, preeclampsia, and other complications requiring specialized pregnancy management.
- Arterial thrombosis: APS can also lead to arterial thrombosis, such as strokes, myocardial infarctions, or peripheral artery thrombosis, which can have serious health consequences for the patient.
- Neurological complications: Some patients with APS may experience various neurological symptoms, including cognitive disturbances, migraines, transient ischemic attacks, or strokes, which require additional attention and monitoring from specialists.
Approaches to the treatment of antiphospholipid syndrome recommended by experts
Experts in the fields of rheumatology and hematology recommend a comprehensive approach to the treatment of antiphospholipid syndrome (APS), which includes both pharmacological and non-therapeutic strategies. The primary goal of treatment is to prevent thrombotic complications and manage other manifestations of APS. An individualized treatment approach is based on the clinical manifestations of the syndrome and the characteristics of the patient, allowing for optimal outcomes and minimizing risks.
Medications include the use of anticoagulants, such as warfarin or heparin, which help prevent the formation of blood clots and reduce the risk of thrombotic complications. Additionally, drugs aimed at improving hemostasis and suppressing the immune response may be used. It is important to emphasize the significance of regular monitoring and assessment of blood parameters in patients with APS for effective management of the condition and timely adjustment of treatment strategies.

Methods for diagnosing antiphospholipid syndrome
Diagnosis of antiphospholipid syndrome (APS) is based on a comprehensive analysis of clinical manifestations, the patient’s history, and the results of specialized laboratory tests. One of the key diagnostic criteria is the detection of elevated levels of antibodies to phospholipids, including anticardiolipin antibodies, antibodies to beta-2-glycoprotein, and lupus anticoagulant. Confirmation of the diagnosis of APS requires the presence of these antibodies in the patient’s blood over an extended period, taking into account the variability of their levels and potential changes due to treatment or other factors.
In addition to laboratory tests, the diagnosis of APS includes imaging studies, such as ultrasound Dopplerography to detect thrombosis, as well as magnetic resonance angiography to assess the condition of the vessels. The clinical manifestations of thromboembolic complications and other aspects of APS also play an important role in establishing the diagnosis and assessing the severity of the patient’s condition, which requires a comprehensive approach and extensive medical examination.
- Laboratory tests for antibodies: An important part of diagnosing APS is the analysis of the level of antibodies to phospholipids, including anticardiolipin antibodies and lupus anticoagulant, conducted through specialized laboratories.
- Coagulation studies: Conducting coagulation tests, such as measuring blood clotting time, helps identify disorders in the coagulation system that may be characteristic of APS.
- Ultrasound Dopplerography: The use of ultrasound dopplerography allows for the detection of thromboses in the venous system, which is one of the characteristic signs of APS.
- Magnetic Resonance Angiography: MR-angiography is used to visualize the condition of blood vessels and identify vascular changes associated with antiphospholipid syndrome.
- Clinical analysis of symptoms: Analyzing the clinical manifestations in the patient, such as thromboses, pregnancy complications, or neurological symptoms, is also an important method for diagnosing and assessing the severity of APS.
Strategies for treating antiphospholipid syndrome
Important aspects of APS treatment also include non-therapeutic strategies, such as controlling risk factors for thrombosis, maintaining a healthy lifestyle, and regular medical check-ups to assess the condition and treatment effectiveness. Patients with APS should seek qualified medical assistance, adhere to prescribed therapy, and participate in preventive measures to reduce the risk of thrombosis and improve the prognosis of the disease.
- Medication therapy: The basis of treating antiphospholipid syndrome is the use of anticoagulants, such as warfarin or low-molecular-weight heparin, to prevent thrombosis and reduce the risk of thrombotic complications.
- Individualized approach: Treatment of APS requires an approach based on clinical manifestations, the presence of comorbidities, and the risk of thrombosis for each patient, which allows for optimizing therapy and treatment outcomes.
- Thrombosis prevention: The use of antiplatelet agents and controlling risk factors for thrombosis, such as smoking, physical inactivity, and obesity, play an important role in preventing thrombotic complications in patients with APS.
- Compliance with treatment: Adhering to the doctor’s recommendations for medication treatment, regular follow-up examinations, and maintaining a healthy lifestyle are fundamental strategies in managing antiphospholipid syndrome.
- Shared management with the patient: Interaction between the physician and the patient, explaining treatment goals, understanding the principles of medication therapy and condition monitoring, contribute to effective control of APS and improve disease prognosis.
Strategies for the prevention of antiphospholipid syndrome
For women with APS, special attention is paid to preventing complications during pregnancy, such as an increased risk of preterm labor or pregnancy loss. Planning pregnancy with consideration of the disease characteristics and regular medical monitoring by specialists helps to prevent complications and ensure a favorable outcome for both mother and child.
- Healthy lifestyle: Adhering to a healthy lifestyle, including regular physical activity, healthy eating, weight management, and avoiding harmful habits, contributes to overall health improvement and reduces the overall risk of thromboses and other complications.
- Reducing risk factors: Controlling risk factors for thrombosis, such as hypertension, dyslipidemia, and diabetes, as well as preventing cardiovascular diseases, helps to decrease the likelihood of thrombosis in patients at increased risk of APS.
- Use of antiplatelet agents: In patients with a history of thrombosis or high risk of thrombosis, the use of antiplatelet agents, such as aspirin, may be recommended to reduce blood clotting and prevent thrombotic complications.
- Adequate management during pregnancy: Planning pregnancy considering the features of APS, regular medical monitoring during pregnancy, and treatment under the supervision of specialists help prevent complications and ensure safe motherhood.
- Patient education: An important aspect of APS prevention is educating patients about the disease, risk factors, the necessity of adhering to prescribed treatment, and regular consultations with doctors for effective prevention of thrombosis and management of the condition.
Amazing features of antiphospholipid syndrome
Another surprising aspect of antiphospholipid syndrome is its association with various autoimmune diseases, such as systemic lupus erythematosus or rheumatoid arthritis. This points to the complex immunopathology underlying the development of APS and highlights the need for a comprehensive approach to the diagnosis and treatment of this syndrome. The rapid advancement of scientific research in the field of antiphospholipid syndrome continues to expand our understanding of this condition and ways to manage it effectively.