Ovarian apoplexy: causes, symptoms, and treatment
- Understanding ovarian apoplexy
- Factors contributing to the development of ovarian apoplexy
- Signs of ovarian apoplexy
- Expert opinion on the treatment of ovarian apoplexy
- Methods of diagnosing ovarian apoplexy
- Methods of treating ovarian apoplexy
- Measures for the prevention of ovarian apoplexy
- Interesting aspects of ovarian apoplexy
- FAQ
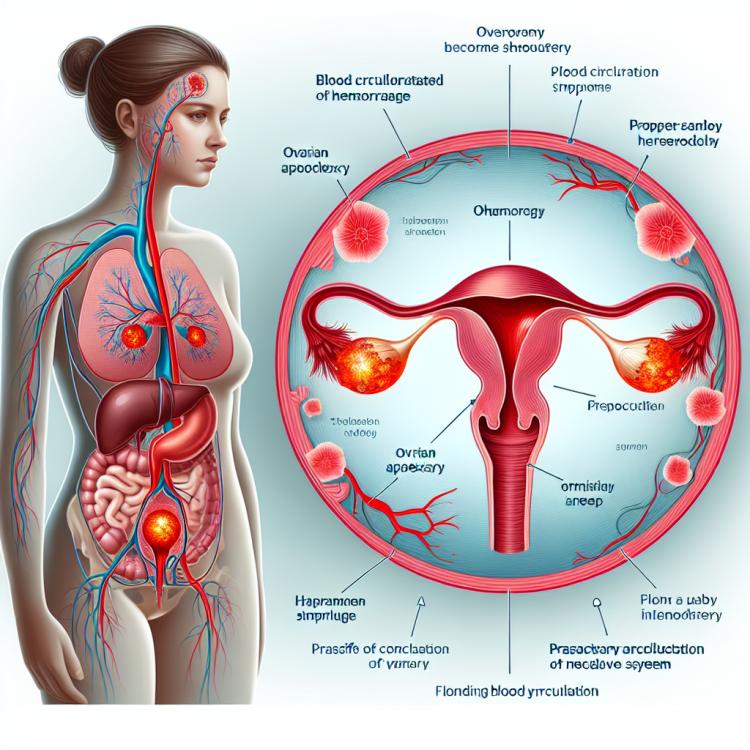
Understanding ovarian apoplexy
Ovarian apoplexy is an acute form of a vascular incident characterized by the rupture of a blood vessel in the ovary. This process is often accompanied by internal bleeding into the abdominal cavity and causes sharp pain in the lower abdomen, more commonly in women of reproductive age. A ruptured vessel can lead to significant blood loss and result in a state of shock, requiring urgent medical attention. Understanding ovarian apoplexy is important for timely diagnosis and appropriate treatment, which may include conservative therapeutic measures or even surgical intervention.
Factors contributing to the development of ovarian apoplexy
Various factors can contribute to the development of ovarian apoplexy. One of the most common causes is the disruption of the integrity of the blood vessels supplying the ovary, which can occur during intense physical exertion, trauma, or other severe circumstances. There are also medical conditions that increase the risk of developing this condition, such as blood clotting disorders or hormonal changes that affect ovarian function. Understanding these factors is essential for the prevention and timely treatment of ovarian apoplexy, which helps reduce potential negative consequences and improve the prognosis for patients.
- Injuries or blows to the abdominal area: mechanical impact on the ovaries can cause blood vessel damage and contribute to the development of ovarian apoplexy.
- Intensive physical activity: overloading the body during sports or other activities can lead to disrupted blood circulation in the ovaries.
- Hormonal disorders: changes in hormone levels, such as polycystic ovary syndrome or irregular cycles, may be associated with the development of ovarian apoplexy.
- Taking certain medications: certain drugs can affect the state of blood vessels and increase the risk of blood vessel rupture in the ovaries.
- Medical procedures or surgical interventions: some medical manipulations, such as ovarian puncture or cesarean section, can increase the likelihood of ovarian apoplexy occurring.
Signs of ovarian apoplexy
Symptoms of ovarian apoplexy may include acute pain in the lower abdomen or pelvic area, which can be severe and sharp. Patients often describe this pain as unlike anything else, and it may be accompanied by nausea, vomiting, and general malaise. Additionally, symptoms of shock may occur, such as pale skin, increased heart rate, low blood pressure, and dizziness, which require immediate medical attention.
Understanding and timely recognition of the signs of ovarian apoplexy play an important role in diagnosing and managing this condition. In case of the aforementioned symptoms, it is important to consult qualified medical professionals for diagnosis, determining the cause, and, if necessary, initiating appropriate treatment.
- Acute pain in the lower abdomen: patients often describe intense sharp pain, unusual for them, occurring in the abdominal or pelvic area.
- Nausea and vomiting: symptoms of dyspepsia, such as nausea and vomiting, may accompany ovarian apoplexy due to blood leakage into the abdominal cavity.
- General malaise: feelings of weakness, fatigue, and general malaise may be observed in patients with ovarian apoplexy due to blood loss and stress on the body.
- Shock syndrome: symptoms of shock, including skin pallor, increased heart rate, decreased blood pressure, and dizziness, may develop in acute ovarian apoplexy and require urgent medical attention.
- Menstrual cycle disturbance: changes in the regularity or intensity of menstruation may be a sign of possible ovarian dysfunction, including the possibility of apoplexy.
Expert opinion on the treatment of ovarian apoplexy
Experts in the field of gynecology pay special attention to the treatment of ovarian apoplexy, striving for a balanced and effective approach. The main methods of treating ovarian apoplexy are conservative therapy and, in some cases, surgical intervention. Conservative treatment often includes the use of anti-inflammatory medications, pain management, and monitoring the patient’s condition to prevent possible complications. In cases where conservative methods are not sufficiently effective or the patient has other complications, surgical intervention may be necessary to address the problem of ovarian apoplexy and restore normal organ function.

Methods of diagnosing ovarian apoplexy
Diagnosis of ovarian apoplexy includes a set of methods aimed at identifying vessel rupture and assessing the condition of the ovary in the patient. Clinical examination and medical history are important primary steps in identifying signs of apoplexy. Additional diagnostic methods may include ultrasound examination of the pelvic organs, which helps determine the presence of internal bleeding, as well as identifying specific changes in the ovary.
In addition to ultrasound, in some cases, computed tomography or magnetic resonance imaging may be required to obtain a more detailed picture of the condition of the ovary and surrounding tissues. Accurate and timely diagnosis of ovarian apoplexy is key to determining treatment measures and preventing possible complications, so medical professionals strive to use all available methods for reliable diagnosis of this condition.
- Clinical examination: the initial stage of diagnosis, including an analysis of the symptoms and medical history of the patient to identify suspicions of ovarian apoplexy.
- Ultrasound examination: a non-invasive method that allows visualization of the pelvic organs, detection of internal bleeding, and changes in the structure of the ovary.
- Computed tomography (CT): performed to obtain more detailed information about the condition of the ovary and surrounding tissues through radiographic imaging using computer processing.
- Magnetic resonance imaging (MRI): a high-precision imaging method that uses a magnetic field to create three-dimensional images that help assess the condition of the ovary.
- Laboratory blood tests: including a complete blood count, hormone level analysis, and coagulogram to assess the patient’s condition and identify blood coagulation disorders.
Methods of treating ovarian apoplexy
The admission of a patient with suspected ovarian apoplexy requires competent and timely assistance from specialized medical services. An individualized approach to treatment is key to successful therapy, as each case requires careful assessment, selection of the optimal method, and monitoring of the patient’s further development.
- Conservative treatment: includes taking anti-inflammatory drugs and analgesics, rest to allow for the healing of torn vessels, as well as monitoring the patient’s condition and symptoms for regular assessment of treatment efficacy.
- Surgical intervention: in cases of severe internal bleeding or ovarian rupture, surgery may be required to remove blood from the abdominal cavity and to restore blood flow to the ovary or even to resect the affected organ.
- Emergency medical care: in cases of suspected ovarian apoplexy, it is essential to immediately seek medical services for qualified assistance and timely initiation of treatment.
- Support of vital functions: in cases of severe condition and risk of complications, it is important to provide support for the patient’s vital functions and pathological changes to minimize potential risks.
- Individualized approach: each case requires treatment and monitoring tailored to the patient, so it is important to consider the specifics of each situation to determine the optimal treatment method and prevention of complications.
Measures for the prevention of ovarian apoplexy
Educating women about the symptoms of reproductive disorders and being attentive to their health allows for the earlier detection of potential problems and seeking specialist advice for further examination and treatment. Timely management of chronic conditions such as endometriosis and polycystic ovary syndrome is also an important part of preventing ovarian apoplexy. In general, systematic measures to monitor the health of the female reproductive system and meticulous observation of possible pathologies contribute to reducing the risk of developing ovarian apoplexy.
- Regular gynecological examinations: periodic check-ups with a specialist help detect ovarian pathologies at an early stage and ensure timely treatment.
- Hormonal background control: maintaining normal hormone levels contributes to the health of the reproductive system and can help prevent potential disorders, including ovarian apoplexy.
- Healthy lifestyle: moderate physical activity, proper nutrition, quitting smoking, and moderate alcohol consumption contribute to the overall health of the female reproductive system.
- Awareness training of symptoms: knowledge of the main manifestations of reproductive disorders will help women pay attention to any changes more quickly and seek medical diagnosis.
- Treatment of chronic diseases: timely and correct treatment of other common gynecological conditions, such as endometriosis and polycystic ovary syndrome, can help prevent complications, including ovarian apoplexy.
Interesting aspects of ovarian apoplexy
Another interesting aspect of apoplexy is the possibility of symptom exacerbation during menstruation in some women. Menstruation can intensify pain and worsen the condition in ovarian apoplexy due to changes in the reproductive system at this time of the menstrual cycle. Such features of the disease highlight the importance of diagnosing and treating ovarian apoplexy while considering the individual characteristics of each patient.