Appendicular infiltrate: symptoms, diagnosis, and treatment
- Understanding appendiceal infiltration
- Factors contributing to the development of appendicular infiltration
- How does appendicular infiltrate manifest?
- Expert opinion on the treatment of appendiceal infiltrate
- Methods for diagnosing appendicular infiltrate
- Appendicular infiltration treatment
- Prevention of appendicular infiltration
- Funny facts about appendicular infiltrate
- FAQ
Understanding appendiceal infiltration
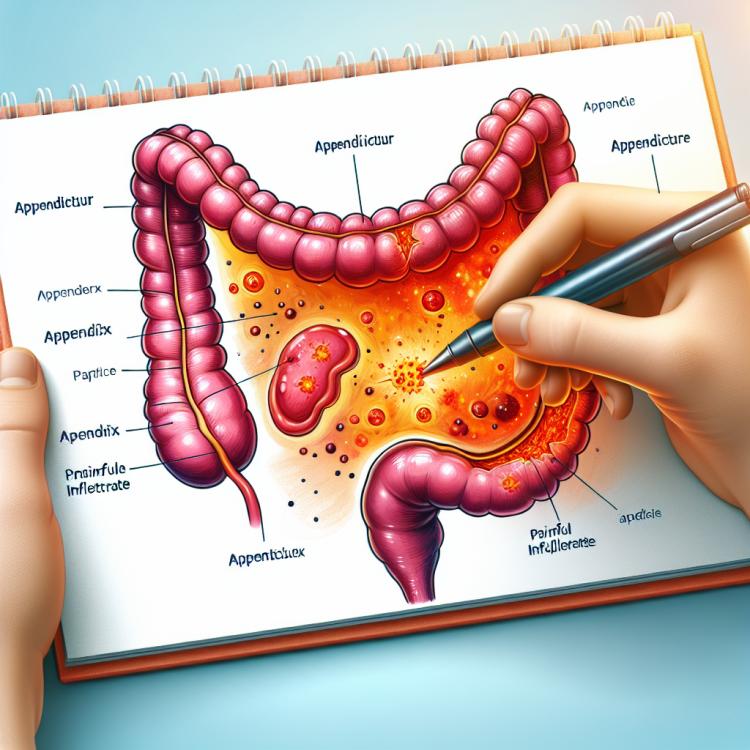
Appendicular infiltrate is an inflammatory condition characterized by the formation of a localized area of inflammation in the region of the appendix. This condition is often caused by the absorption of infectious material into the appendiceal process following an infection of the appendix. Symptoms include pain in the right lower quadrant of the abdomen, vomiting, fever, and changes in the white blood cell count.
The diagnosis of appendicular infiltrate often includes physical examination, laboratory studies (such as a complete blood count for inflammation), and instrumental methods, including ultrasound and computed tomography. Treatment can range from conservative methods, such as antibiotics, to surgical intervention depending on the clinical picture and the severity of the patient’s condition.
Factors contributing to the development of appendicular infiltration
The development of an appendiceal infiltrate may be due to various factors, including the complicated nature of appendicitis or insufficient or untimely treatment of acute appendicitis. Some patients may have a higher risk of developing an infiltrate due to late presentation for medical help, leading to a prolonged period of inflammation before an accurate diagnosis is established.
Other possible causes include young age, the presence of risk factors for the development of acute appendicitis, such as appendiceal colic, and abnormalities in the structure of the appendix that may contribute to its inflammation and the formation of an infiltrate. Understanding these factors and risks helps in determining treatment strategies and managing cases of appendiceal infiltrate.
- Residual infection: Untimely or incomplete treatment of acute appendicitis may lead to the formation of an appendiceal infiltrate.
- Pre-granulomatous nature of appendicitis: Complications in the course of acute appendicitis may contribute to the formation of an infiltrate around the appendix.
- Late seeking of medical assistance: Prolonged inflammation without adequate treatment can lead to the formation of an infiltrate.
- Young age: Young individuals may have more pronounced reactions to infections, which can increase the risk of developing an appendiceal infiltrate.
- Anomalies in the structure of the appendix: Some anomalies in the structure of the appendix may contribute to its inflammation and the formation of an infiltrate.
How does appendicular infiltrate manifest?
Appendicular infiltrate usually manifests with clinical symptoms, including pain in the lower right quadrant of the abdomen, which may intensify upon palpation or movement; bowel disturbances such as diarrhea or constipation; nausea and vomiting; and an increase in body temperature, especially in the case of a complicated condition. Patients may also show changes in the leukocyte formula, indicating an inflammatory process in the body.
The diagnosis of appendicular infiltrate typically involves examining the patient, laboratory studies such as a complete blood count and urinalysis, and instrumental methods such as ultrasound or computed tomography. Considering the characteristic clinical and laboratory picture, doctors can make a preliminary diagnosis of appendicular infiltrate and determine the necessity for conservative or surgical treatment.
- Pain in the right lower quadrant of the abdomen: The characteristic pain may be sharp, acute, and increase with pressure or movement.
- Bowel disturbances: Patients with appendicular infiltrate may experience changes in bowel function, such as diarrhea or constipation.
- Nausea and vomiting: Symptoms may be accompanied by feelings of nausea and vomiting, especially during a prolonged inflammatory process.
- Fever: Acute inflammation around the appendix may cause fever and elevated body temperature.
- Changes in the white blood cell count: Laboratory tests may show an increase in the number of white blood cells, indicating the presence of an inflammatory process in the body.
Expert opinion on the treatment of appendiceal infiltrate
Experts in medicine agree that the treatment of appendicular infiltrate should be individualized and determined by the clinical manifestations of each specific case. In some instances, especially when minimal symptoms and exacerbations are present, conservative treatment using antibiotics may be sufficient for resorption of the inflammatory focus. However, in cases of acute clinical presentation and complications, doctors more often resort to surgical intervention to evacuate the contents of the infiltrate and prevent possible complications such as perforation of the appendix or peritonitis.
Experts also emphasize the importance of seeking medical help in a timely manner when suspecting an appendicular infiltrate, as delays in diagnosis and treatment can lead to further complications and an increased risk of surgical intervention. A comprehensive approach to treatment, based on a thorough assessment of the clinical picture and individual characteristics of the patient, allows experts to make informed decisions about the choice of the optimal treatment strategy for appendicular infiltrate.

Methods for diagnosing appendicular infiltrate
The diagnosis of appendiceal infiltrate involves a comprehensive use of various methods to determine the presence and characteristics of the inflammatory focus in the area of the appendix. A physical examination of the patient, taking into account complaints and typical symptoms, is the first stage of diagnosis. In addition, laboratory tests such as a complete blood count with close attention to changes in the leukocyte formula and C-reactive protein can provide insight into the presence of inflammation in the body.
Instrumental methods, such as ultrasound and computed tomography, are widely used to visualize the area of the appendix and determine the nature of the infiltrate. Ultrasound allows for the assessment of structural changes and the presence of fluid or tumors in the area of the appendix, while computed tomography provides a more detailed image and can help in the differential diagnosis with other pathologies of the abdominal cavity. The combined use of various diagnostic methods allows for a more accurate determination of the patient’s condition and the decision on the necessity of conservative or surgical treatment.
- Physical examination: The doctor examines the patient, paying attention to the characteristics of the pain, the point of tenderness, and other clinical signs of appendiceal infiltration.
- Laboratory blood tests: A complete blood count may show an increase in white blood cells and C-reactive protein, indicating the presence of an inflammatory process in the body.
- Ultrasound examination: Allows visualization of the appendiceal area and determination of the presence of fluid, tumors, or other changes in the structure of the appendix.
- Computed tomography (CT): Provides detailed imaging of the abdominal cavity, allowing for the characterization of the infiltration and exclusion of other pathologies.
- Diagnostic laparoscopy: An invasive method that may be used to visualize the area of the appendix and clarify the diagnosis, especially in complex cases.
Appendicular infiltration treatment
However, in cases of acute clinical symptoms, the presence of perforation of the appendix, or other complications, surgery is usually required. Surgery may involve removing the infiltration or the appendix, draining and cleaning the abdominal cavity of pus or other fluids. A comprehensive treatment of appendicular infiltration requires an individual approach and coordination between medical and surgical therapy.
- Conservative treatment with antibiotics: The use of antibiotics is aimed at reducing inflammation and controlling infection, facilitating the resorption of the infiltrate without surgical intervention.
- Drainage of the infiltrate: In the case of abscess formation or significant pus presence, drainage can help in removing discharge and improving the patient’s condition.
- Surgical removal of the appendix: In cases of acute infiltrative form, gangrene of the appendix, or other complications, surgical intervention to remove the appendix may be necessary.
- Laparoscopic intervention: Minimally invasive surgery may be applied to remove the infiltrate through small incisions, contributing to a faster recovery for the patient.
- Monitoring and rehabilitation: After any treatment method, it is important to monitor the patient, track the healing process, and provide necessary medical support for complete recovery.
Prevention of appendicular infiltration
Preventing perforation of the appendix is also important for the prevention of appendicular infiltration. Quickly seeking medical help when characteristic symptoms appear, including pain in the right lower quadrant of the abdomen, nausea, and vomiting, helps prevent acute and complicated forms of appendicitis that can lead to infiltration. Regular medical check-ups and paying close attention to one’s health help identify potential problems in time and prevent their development.
- Maintaining a healthy lifestyle: Leading an active lifestyle, monitoring weight, and proper nutrition contribute to the overall strengthening of the body and reduce the risk of inflammatory processes.
- Regular consumption of high-fiber foods: Including fruits, vegetables, grains, and other fiber-rich products in the diet helps maintain healthy bowel function and prevents possible inflammation.
- Maintaining regular physical activity: Moderate physical exercise helps improve blood circulation, overall body health, and reduce the risk of inflammatory processes in the abdominal organs.
- Timely seeking medical help when acute appendicitis symptoms are suspected: Quick identification and treatment of acute appendicitis help prevent the development of complications, including appendiceal infiltrate.
- Regular medical check-ups: Conducting periodic medical examinations will help identify potential problems with the appendix at an early stage and take measures to prevent possible complications.
Funny facts about appendicular infiltrate
An interesting fact is that appendicular infiltrate can sometimes be observed in patients who initially did not pay attention to mild symptoms of acute appendicitis and delayed their visit to the doctor. Therefore, in the early stages, even minor abdominal complaints should be taken seriously to avoid the development of an infiltrate and prevent possible complications.