Arthrosis: causes, symptoms, and treatment methods
- Definition of osteoarthritis
- Factors contributing to the development of osteoarthritis
- Manifestations of osteoarthritis
- Expert opinion on the treatment of osteoarthritis
- Methods for diagnosing osteoarthritis
- Methods of treating osteoarthritis
- Prevention measures for osteoarthritis
- Interesting facts about osteoarthritis
- FAQ
Definition of osteoarthritis
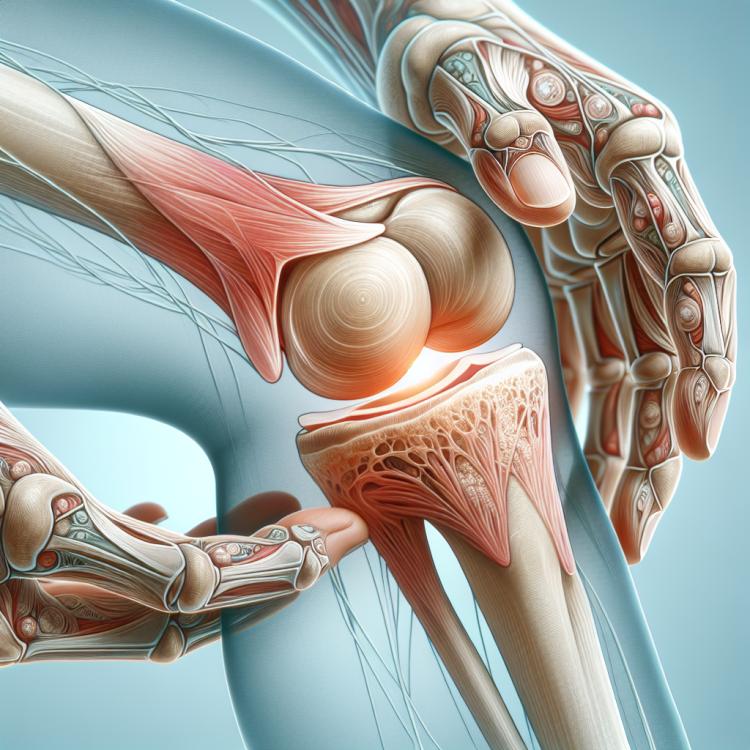
Arthrosis is a chronic joint disease characterized by dystrophic changes in the cartilage tissue, as well as damage to the surrounding tissues and structures of the joint. The pathological process of arthrosis leads to the gradual destruction of cartilage and the formation of osteophytes, resulting in decreased joint mobility and pain sensations in patients.
The development of arthrosis is usually associated with risk factors such as age, genetic predisposition, joint overloads, injuries, structural anomalies of the joints, and obesity. The diagnosis of arthrosis is based on the medical history, the characteristics of clinical symptoms, the results of joint examination, and the formation of X-ray images to determine the degree of joint damage.
Factors contributing to the development of osteoarthritis
The development of osteoarthritis is caused by various factors, including age-related changes, genetic predisposition, joint overload, injuries, and anomalies in joint structure. In the aging process, cartilage tissue loses its elasticity and ability to recover, which contributes to the progression of degenerative changes in the joints.
Genetic factors can play a significant role in the tendency to develop osteoarthritis, influencing the structure and function of cartilage. Additionally, injuries, damage to joints, improper distribution of loads on certain joints, and excess weight can also contribute to the development of osteoarthritis and accelerate the progression of the disease.
- Age: As one ages, the cartilage loses its elasticity, which contributes to the development of degenerative changes in the joints.
- Genetic predisposition: Hereditary factors can influence the structure and function of cartilage, increasing the risk of developing osteoarthritis.
- Joint overloads: Excessive physical activity or long-term strain can lead to cartilage damage and the development of osteoarthritis.
- Injuries and joint damage: Repeated injuries or serious damage to the joints can accelerate the process of cartilage destruction and the onset of osteoarthritis.
- Excess weight: Obesity exerts additional pressure on the joints, which can contribute to their wear and the development of osteoarthritis.
Manifestations of osteoarthritis
Symptoms of osteoarthritis often include pain in the affected joint, which can intensify with movement or physical activity. Patients may also experience stiffness and limited mobility of the joint due to degenerative changes in the cartilage and surrounding tissues. Morning stiffness and difficulties with initiating movement in the joint are also characteristic of osteoarthritis.
In addition to pain and limited mobility, symptoms of osteoarthritis may include joint inflammation, swelling, and sometimes the formation of osteophytes. Patients may experience increasing weakness in the affected joint, as well as signs of deformity or changes in the appearance of the joint as the disease progresses.
- Pain sensations: Characterized by joint pain that may increase with movement or physical activity.
- Movement restriction: Patients may experience stiffness and difficulty fully performing movements due to cartilage deformation and surrounding tissue.
- Morning stiffness: A feeling of stiffness in the joint in the morning, which passes after some time of activity.
- Inflammation and swelling: Some cases of osteoarthritis may be accompanied by joint inflammation and swelling in the affected area.
- Weakness and deformation: Progressive osteoarthritis may cause a feeling of weakness in the joint and observable deformation or changes in the appearance of the affected joint.
Expert opinion on the treatment of osteoarthritis
Experts in the field of rheumatology and orthopedics emphasize the importance of a comprehensive approach to treating osteoarthritis, which includes non-drug methods, pharmacological therapy, physiotherapy, and, if necessary, surgical intervention. An individualized approach to each patient, taking into account the stage of disease development, its characteristics, and accompanying factors, is a key aspect of effective osteoarthritis treatment.
Experts highlight the significance of regular monitoring of the patient’s condition during treatment and adapting therapy based on dynamics. An important component is educating the patient on self-management, including recommendations for physical activity, weight control, and the use of assistive devices. Furthermore, experts stress the necessity of long-term supportive treatment to control symptoms and maintain joint functionality in patients with osteoarthritis.

Methods for diagnosing osteoarthritis
Various methods are used for the diagnosis of osteoarthritis, starting with a comprehensive history and physical examination of the patient. X-ray remains one of the main examination methods, allowing visualization of the degree of degenerative changes in the joints, the presence of osteophytes, and deterioration of the cartilage structure. In addition, in some cases, magnetic resonance imaging (MRI) or computed tomography (CT) may be used to obtain more detailed information about the condition of the joints and surrounding tissues.
Additional diagnostic methods for osteoarthritis may include laboratory tests to exclude other possible causes of joint pain, such as inflammatory diseases. Joint examination through arthroscopy may be used for a more accurate determination of the extent of damage and planning further therapeutic interventions.
- Anamnesis and physical examination: Conducting a conversation with the patient and examining the joints to identify characteristic signs such as pain, stiffness, swelling, and limited mobility.
- X-ray: Radiological examination that allows visualization of degenerative changes, presence of osteophytes, and condition of cartilage tissue in the affected joints.
- Magnetic resonance imaging (MRI): A more detailed non-invasive examination of the joints to identify changes in soft tissues, cartilage, and bone structure.
- Computed tomography (CT): Visualization of the joints using X-rays and computer processing to obtain a three-dimensional image of the details of the damage.
- Laboratory studies: Blood tests and joint fluid analysis can help rule out other inflammatory processes and confirm the diagnosis of osteoarthritis.
Methods of treating osteoarthritis
In cases where conservative methods are not sufficiently effective, surgical intervention may be required. Surgical treatment of osteoarthritis can include arthroscopy, arthrodesis, resection, or joint replacements. The decision about the treatment method depends on the extent of changes in the joint, the overall condition of the patient, and their individual characteristics.
- Physical therapy: A set of exercises and procedures aimed at improving joint mobility, strengthening muscles, and reducing joint pain.
- Pharmacological therapy: The use of anti-inflammatory drugs, painkillers, and chondroprotectors to reduce inflammation and symptoms of osteoarthritis.
- Injections: Administration of medications into the joint to reduce pain and inflammation, such as glucocorticoids and hyaluronic acid.
- Surgical intervention: In advanced stages of osteoarthritis, surgery may be required, including arthrodesis, arthroplasty, or joint replacement.
- Physiotherapy: The application of techniques such as ultrasound, laser therapy, and magnetotherapy to improve blood circulation, relieve inflammation, and enhance joint function.
Prevention measures for osteoarthritis
Other important preventive measures include proper distribution of physical load, avoiding traumatic situations, giving up harmful habits such as smoking, and regular medical check-ups to timely detect and monitor the early signs of arthrosis. Providing joints with proper support and protection while performing daily tasks and sporting activities also helps reduce the likelihood of developing degenerative changes and maintain the functionality of the joints in the long term.
- Regular physical exercise: Moderate physical activity, including strengthening exercises, helps maintain muscle tone and joint flexibility, reducing the risk of developing osteoarthritis.
- Maintaining a healthy weight: Excess weight puts extra stress on the joints, so controlling body mass through healthy eating and regular physical activity helps prevent the development of osteoarthritis.
- Avoiding injuries and overloads: Preventing traumatic damage to the joints, distributing physical loads properly, and avoiding overloads will help maintain joint health in the long run.
- Quitting harmful habits: Many harmful habits, such as smoking, can negatively affect joint health and contribute to the development of osteoarthritis. Quitting such habits is an important preventive measure.
- Regular medical check-ups: It is important to have regular medical check-ups to timely identify early changes in the joints and discuss preventive measures with a doctor.
Interesting facts about osteoarthritis
Another interesting fact is that osteoarthritis is not just “wear and tear” that inevitably comes with age, but a complex disease associated with biochemical and structural changes in the joints. Studying the molecular mechanisms of osteoarthritis development will help in developing more effective methods for the diagnosis and treatment of this disease.