Osteoarthritis of the shoulder joint: development mechanism, prevention, and modern treatment methods
- Understanding shoulder joint osteoarthritis
- Etiology of shoulder joint osteoarthritis
- Clinical picture of shoulder joint osteoarthritis
- The specialists’ perspective on the therapy for shoulder joint osteoarthritis
- Methods of diagnosing shoulder joint osteoarthritis
- Approaches to the treatment of shoulder joint arthrosis
- Prevention of shoulder joint osteoarthritis
- Interesting aspects of shoulder joint osteoarthritis
- FAQ
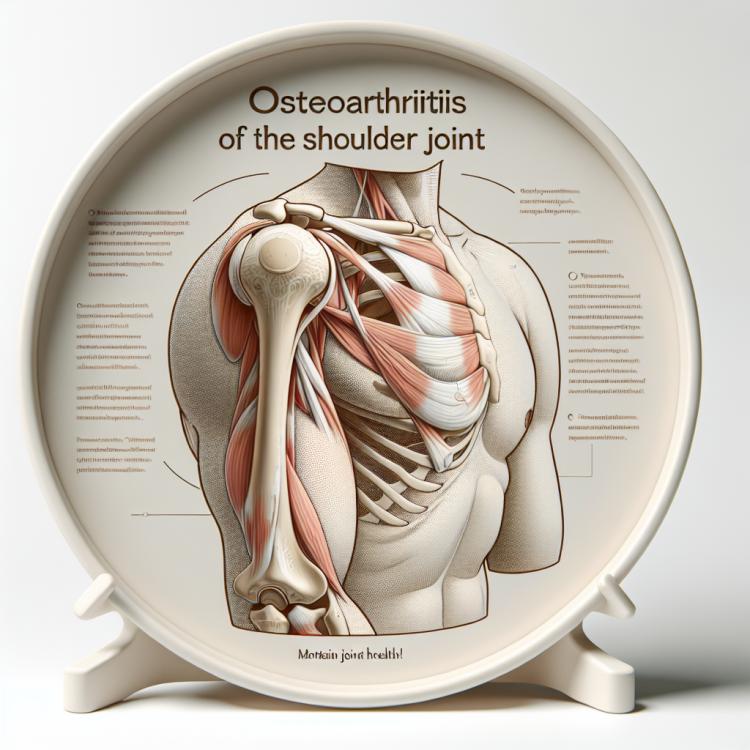
Understanding shoulder joint osteoarthritis
Shoulder osteoarthritis is a degenerative disease characterized by the gradual destruction of cartilage tissue in the joint. This condition is usually accompanied by pain, limited movement, and a deterioration in the patient’s quality of life. Risk factors for developing shoulder osteoarthritis include aging, injuries, genetic predisposition, and increased joint load.
To diagnose shoulder osteoarthritis, physical examinations, X-rays, and other diagnostic procedures are conducted. Treatment for shoulder osteoarthritis typically includes conservative methods such as physical therapy, medication therapy, and exercises to strengthen the muscles. In some cases, surgical intervention may be required to improve joint function and relieve osteoarthritis symptoms.
Etiology of shoulder joint osteoarthritis
Osteoarthritis of the shoulder joint is a chronic degenerative disease characterized by deformation of the joint surfaces, damage to the cartilage tissue, and inflammation of the surrounding tissues. One of the main causes of shoulder osteoarthritis is natural aging, which leads to the wear of cartilage due to constant loads and mechanical impact on the joint. Risk factors for the development of shoulder osteoarthritis can also include mechanical injuries, posture disorders, congenital joint anomalies, as well as exogenous factors, including excess weight and poor nutrition.
- Aging: The accumulation of damage in the cartilage due to natural wear over time is one of the main causes of shoulder osteoarthritis.
- Mechanical injuries: Traumatic injuries such as fractures, dislocations, and sprains can contribute to the development of shoulder osteoarthritis.
- Incorrect posture: Prolonged maintenance of poor posture can lead to uneven distribution of loads on the joint, which promotes the development of osteoarthritis.
- Congenital joint anomalies: The presence of deformities or underdevelopment of joint structures from birth may increase the risk of developing shoulder osteoarthritis.
- Excess weight: Increased load on the joints due to excess weight can contribute to cartilage degeneration and the development of shoulder osteoarthritis.
Clinical picture of shoulder joint osteoarthritis
Osteoarthritis of the shoulder joint manifests with various clinical symptoms, including pain syndrome, limited mobility in the joint, creaking and crunching during movements, as well as swelling and increased joint volume. Patients often note increased pain during physical activity and loads on the shoulder girdle, which can lead to a limitation of everyday movements and a decline in quality of life. Additionally, in shoulder joint osteoarthritis, muscular weakness and atrophy of the shoulder muscles frequently occur, further aggravating functional impairments and reducing the overall physical activity of the patient.
- Pain syndrome: patients often experience pain in the shoulder joint, which can be chronic or worsen with physical activity.
- Limited mobility: shoulder joint osteoarthritis is often accompanied by a decrease in the range of motion in the joint, making it difficult to perform daily tasks.
- Creaking and crunching: during movements in the shoulder joint, patients may hear characteristic sounds related to the wear of the cartilage tissue.
- Swelling and increased joint volume: inflammatory processes in the joint can lead to swelling and an increase in the volume of the joint tissues.
- Muscle weakness and atrophy: as a result of limited movement and pain syndrome, muscle weakness and atrophy of the shoulder muscles may develop, further worsening the condition of the joint.
The specialists’ perspective on the therapy for shoulder joint osteoarthritis
Experts in orthopedics and rheumatology emphasize the importance of a comprehensive approach to the treatment of shoulder joint osteoarthritis, which includes conservative methods such as physical therapy, medication therapy, and exercise, as well as surgical interventions when necessary. There is consensus that early detection of shoulder osteoarthritis and timely initiation of treatment contribute to more successful outcomes and improved disease prognosis.
Experts also highlight the importance of an individualized approach to treatment, taking into account the characteristics of each patient, the stage of the disease, and the presence of comorbid processes and disorders. Specialists recommend regular monitoring of the patient’s condition, adjusting therapy based on the dynamics of the disease, and adhering to rehabilitation recommendations to achieve optimal results in the treatment of shoulder joint osteoarthritis.

Methods of diagnosing shoulder joint osteoarthritis
Various methods are used to diagnose shoulder joint osteoarthritis, including clinical examination, X-ray, magnetic resonance imaging (MRI), and computed tomography (CT). Clinical examination allows for the identification of characteristic symptoms of osteoarthritis, such as pain in the shoulder area, limited mobility, and crepitus during movements. X-ray is widely used to visualize changes in the joint structure, such as narrowing of the joint space, osteophytes, and sclerosis. MRI and CT allow for a more detailed study of the condition of the joint tissues, revealing possible damage to the cartilage, bone tissue, and surrounding soft tissues.
- Clinical examination: the doctor examines the patient, identifies characteristic symptoms of osteoarthritis, assesses the mobility and tenderness of the joint.
- X-ray: this method allows for visualization of changes in the joint structure, such as narrowing of the joint gap, presence of osteophytes, and sclerosis of the bones.
- Magnetic resonance imaging (MRI): this is a highly accurate imaging method that provides detailed images of the joint tissues, helping to identify cartilage damage and other pathologies.
- Computed tomography (CT): this method allows for obtaining a series of high-resolution slices of the joint, detecting changes in the bone tissue and joint structure.
- Laboratory tests: although it cannot be used for accurate diagnosis of osteoarthritis, laboratory tests can help exclude other inflammatory processes and systemic diseases.
Approaches to the treatment of shoulder joint arthrosis
- Physical therapy: Includes exercises to strengthen shoulder muscles, increase joint mobility, and reduce pain.
- Medication therapy: Involves the prescription of anti-inflammatory drugs, chondroprotectors, analgesics for pain relief, and other medications.
- Physiotherapy: Includes the use of treatment methods such as ultrasound, laser therapy, and magnetotherapy, which help to reduce pain and inflammation.
- Taking dietary supplements: Some patients may take supplements like glucosamine and chondroitin to support the health of cartilage tissue.
- Surgical intervention: In extreme cases, when conservative methods do not lead to improvement, surgical treatment, such as joint replacement, may be recommended.
Prevention of shoulder joint osteoarthritis
- Keep track of your weight and maintain a healthy lifestyle, as excess weight puts additional strain on the joints and can accelerate the development of osteoarthritis.
- Engage in regular exercises to strengthen muscles and maintain flexibility in the shoulder girdle, which helps prevent degenerative changes in the joints.
- Avoid repetitive movements and prolonged sitting in a fixed position to reduce the risk of overloading and injuring the joints.
- Maintain proper posture and pay attention to the position of your shoulders while working at a desk or computer to avoid excessive strain on the joints and shoulder muscles.
- Do not lift heavy objects unnecessarily and use proper technique when lifting items to prevent injuries and excessive strain on the shoulder joint.
Interesting aspects of shoulder joint osteoarthritis
Another interesting aspect of shoulder joint arthrosis is its connection with external factors, such as lifestyle and professional activity. For example, intense physical strain on the shoulder girdle or improper posture while working at a computer can contribute to the development of the disease. Understanding these aspects allows for the development of individual strategies for the prevention and treatment of shoulder joint arthrosis, taking into account the peculiarities of each patient.