Atopic dermatitis: symptoms, diagnosis, and treatment methods
Basics of atopic dermatitis
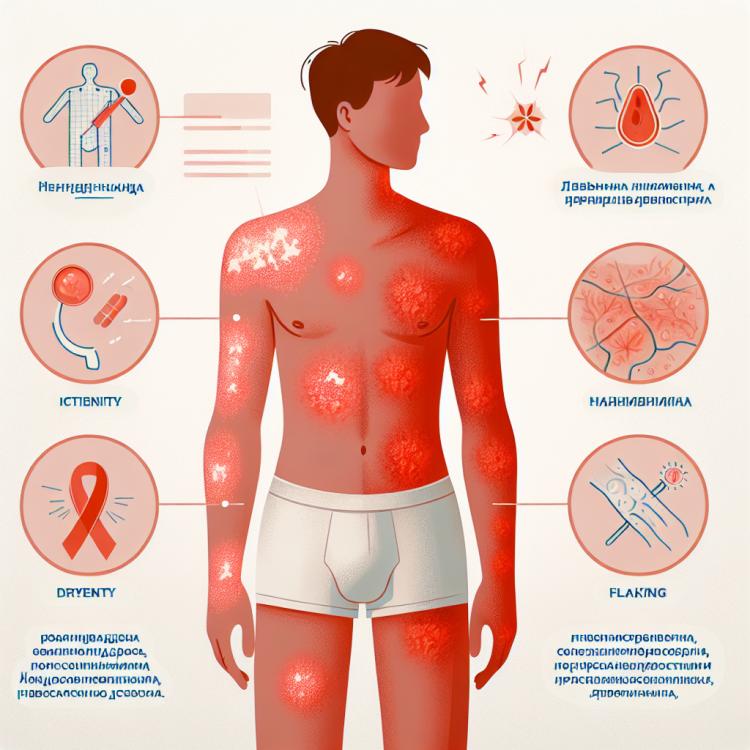
Atopic dermatitis is a chronic inflammatory skin disease, often seasonal, predominantly occurring in childhood. Its main manifestations include itching rash, dry skin, redness, and peeling. In atopic dermatitis, there is a disruption of the protective functions of the epidermis, leading to increased skin sensitivity to irritants.
The diagnosis of atopic dermatitis is based on the clinical picture as well as medical history data. Treatment involves a comprehensive approach, including the use of gentle moisturizers, creams and ointments, anti-inflammatory medications, as well as monitoring factors that contribute to the worsening of skin condition.
Etiology of atopic dermatitis
Atopic dermatitis is a chronic inflammatory skin disease caused by a complex interaction of genetic, immunological, and environmental factors. Genetic predispositions, such as the presence of atopic diseases in relatives, play an important role in the onset of the disease. Among the key factors contributing to the development of atopic dermatitis are the imbalance in the immune system, disruptions in the epidermal barrier of the skin, allergic reactions to external allergens and irritants.
- Genetic factors: The presence of family atopic diseases increases the risk of developing atopic dermatitis.
- Immunological disorders: An imbalance in the body’s immune system can lead to skin inflammation.
- Disruption of the epidermal barrier: A weak skin protective barrier facilitates the penetration of allergens and irritants.
- Allergic reactions: Increased skin sensitivity to various allergens can trigger inflammatory processes.
- Environmental influences: Air pollutants, climatic conditions, and other factors can also contribute to the development of atopic dermatitis.
The clinical picture of atopic dermatitis
The clinical picture of atopic dermatitis often includes characteristic symptoms such as itching, redness of the skin, dryness, and peeling. Patients frequently face exacerbations of the disease, which can manifest as an increase in symptoms, including the appearance of rashes, cracks, and blisters, especially on the flexural areas of the body, such as elbows and knees. More severe cases of atopic dermatitis may be accompanied by wet phenomena and the risk of secondary infection, which requires a comprehensive approach to treatment and management of the disease.
- Itching and discomfort: One of the most characteristic symptoms of atopic dermatitis is the unpleasant feeling of itching, which can be intense and interfere with the patient.
- Redness and inflammation: As the disease progresses, the skin becomes red and inflamed, which is associated with a chronic inflammatory process.
- Dryness and peeling: The skin becomes dry and often peels, which can create additional discomfort for the patient.
- Rashes, blisters, cracks: Various rashes, blisters, and cracks may appear on the skin, especially in the folds of the body, which exacerbates the symptoms of the disease.
- Moist phenomena and risk of secondary infection: In cases of severe atopic dermatitis, moist phenomena are observed on the skin, which can contribute to the development of secondary infection and require special attention during treatment.
Experts’ views on the therapy of atopic dermatitis
The treatment of atopic dermatitis is based on a comprehensive approach that includes the use of moisturizing and anti-inflammatory ointments, hormonal medications during flare-ups, antihistamines to relieve itching, as well as skin care recommendations. Experts emphasize the importance of a personalized approach to treatment, taking into account the patient’s age, the severity of the disease, and the presence of concomitant pathologies, in order to achieve the best results.
Additionally, specialists highlight the significance of educating patients on self-monitoring methods for the disease, warning against potential complications and supporting the patient in maintaining a stable remission. Innovative techniques such as phototherapy or immunomodulating medications may also be included in the treatment plan based on the individual characteristics of each case.

Examination of atopic dermatitis
The diagnosis of atopic dermatitis typically involves a careful medical examination of the skin, assessment of typical symptoms and dermatological manifestations. For differential diagnosis and clarification of the severity of the disease, additional laboratory and instrumental studies may be required, such as blood tests, pathological examination of biopsy material from the affected area of skin, as well as allergy tests to identify sensitivity to potential allergens.
Although the diagnosis of atopic dermatitis is usually based on clinical signs and the patient’s history, a complete assessment of the skin condition and causal factors helps to determine the optimal treatment plan. Early detection and accurate diagnosis of the disease play a crucial role in the effectiveness of treatment and prevention of complications, providing patients with atopic dermatitis competent and targeted medical intervention.
- Skin medical examination: the doctor conducts a detailed examination of the skin to identify characteristic symptoms of atopic dermatitis.
- Blood tests: laboratory tests can help assess the level of inflammation and allergic reactions in the patient’s body.
- Pathomorphological examination: a biopsy of the affected skin allows for an accurate diagnosis and differential diagnosis with other dermatological diseases.
- Allergy tests: conducting allergy tests helps determine sensitivity to allergens that may exacerbate the symptoms of atopic dermatitis.
- Instrumental studies: to assess the condition of the skin and the severity of the disease, instrumental studies such as dermatoscopy or electron microscopy may be required.
Methods of treating atopic dermatitis
- Topical medications: Includes the use of gentle moisturizing creams and ointments to improve skin condition and alleviate symptoms.
- Glucocorticoids: Used to reduce inflammation and itching on the skin during flare-ups of atopic dermatitis.
- Anti-inflammatory medications: Help to reduce inflammatory reactions in the affected skin areas, improving their condition.
- Immunomodulators: Used to correct the body’s immune response and reduce the inflammatory reaction on the skin.
- Phototherapy: A therapeutic method based on exposure to ultraviolet light on the skin, which can be effective in treating atopic dermatitis, especially in severe cases.
Prevention of atopic dermatitis
- Proper skin care: regular moisturizing and using gentle cleansers help maintain the skin’s natural barrier and prevent dehydration.
- Avoiding contact with allergens: identifying and minimizing contact with potential allergens such as dust, pollen, mold, certain foods, or furry animals.
- Maintaining skin hydration levels: hydrated skin is less prone to dryness, itching, and irritation, so using moisturizers contributes to skin health.
- Wearing soft natural clothing: avoiding friction and irritation from synthetic fabrics can reduce the risk of exacerbating atopic dermatitis symptoms.
- Moderate physical activity and healthy eating: a healthy lifestyle strengthens the immune system and overall body condition, including the skin, which can also help in the prevention of atopic dermatitis.
Amazing aspects of atopic dermatitis
Additionally, there is increasing research attention on the role of the skin microbiome in the development of atopic dermatitis. An imbalance of the skin’s bacterial flora may play a significant role in disease exacerbations and chronicity. Understanding the relationships between the microbiome and skin condition opens new perspectives for innovative approaches to the treatment and prevention of atopic dermatitis.