Atrioventricular block: symptoms, types, and possible complications
- Understanding Atrioventricular Blockade
- Etiology of Atrioventricular Block
- Clinical picture of Atrioventricular block
- Views of specialists on the treatment of Atrioventricular block
- Methods for diagnosing Atrioventricular block
- Approaches to the treatment of Atrioventricular block
- Prevention measures of Atrioventricular block
- Amazing aspects of Atrioventricular block
- FAQ
Understanding Atrioventricular Blockade
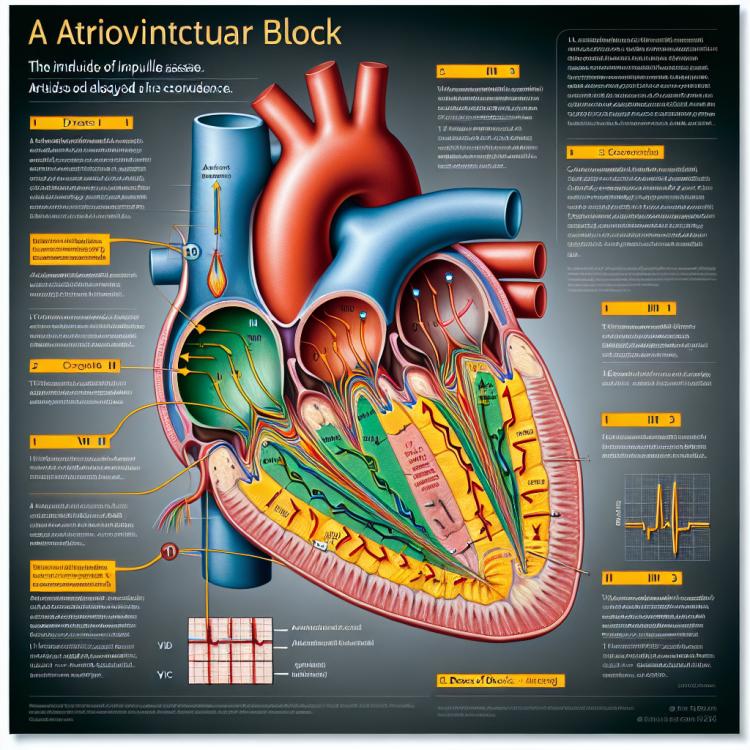
Atrioventricular block is a disturbance in the conduction of impulses from the atria to the ventricles of the heart through the atrioventricular node. This condition can arise due to various heart pathologies, such as myocardial infarction, cardiomyopathy, or age-related changes. The clinical manifestations of AV block range from mild asymptomatic forms to severe cases requiring immediate medical intervention.
Etiology of Atrioventricular Block
Atrioventricular blockade can have various causes, including decreased conduction in the heart’s conduction pathways, ischemic changes in the myocardium, conduction disorders due to congenital heart development anomalies, and nauseous or toxic effects on the heart. These factors can lead to the slowing or blocking of impulse transmission between the atria and ventricles of the heart, which can cause cardiac arrhythmias and other heart problems in patients. An important aspect is identifying the underlying cause of AV blockade in each specific case, allowing for the selection of the most effective treatment plan and subsequent monitoring of the patient’s condition.
- Heart diseases: atrioventricular block can be caused by ischemic heart disease, cardiomyopathies, or other pathologies affecting cardiac conduction.
- Congenital heart anomalies: developmental anomalies of the heart can lead to disruptions in the conduction of electrical impulses and the occurrence of blockages.
- Toxic effects: certain medications, poisons, or toxins can have a negative impact on the cardiac conduction system and cause blockages.
- Metabolic disorders: an imbalance of electrolytes such as potassium, sodium, or magnesium can affect the conductivity of cardiac tissue and may provoke atrioventricular block.
- Aging changes: the aging of cardiac tissue and vessels, as well as degenerative processes, can lead to disruptions in conductivity and the occurrence of conduction pathway blocks.
Clinical picture of Atrioventricular block
Atrioventricular block manifests with various clinical symptoms, depending on the degree of the block and its impact on cardiac activity. Patients may experience feelings of weakness, dizziness, palpitations, shortness of breath, discomfort in the chest, rapid pulsation, or even fainting. In cases of pronounced atrioventricular block, especially with a reduction in the number of impulses conducted to the ventricles of the heart, heart rhythm may be disrupted, which can lead to heart failure and other serious complications.
The diagnosis of atrioventricular block includes clinical examination, ECG, Holter monitoring, and electrophysiological study of the heart. Understanding the type and degree of blockade is crucial for patient management, and in some cases, the placement of an artificial pacemaker may be required to maintain normal heart rhythm and function. In the event of symptoms related to atrioventricular block, it is important to consult a doctor for further examination and treatment.
- Weakness: patients with AV block often complain of general weakness and fatigue due to disturbances in cardiac conduction and circulation.
- Dizziness: episodes of dizziness may occur due to disruptions in blood and oxygen supply to the brain.
- Shortness of breath: breathing difficulties may manifest during physical exertion due to reduced blood supply and oxygen in the tissues.
- Palpitations: patients may experience irregular heartbeats, a feeling of heart interruptions, or arrhythmia as a result of conduction disturbances in the heart.
- Fainting: in cases of severe AV block, fainting may occur due to a significant deterioration in the conduction of cardiac impulses.
Views of specialists on the treatment of Atrioventricular block
Experts in the field of cardiology agree on the importance of an individualized approach to the treatment of atrioventricular block, depending on the type of block, symptoms, and the patient’s condition. Treatment strategies may include observation, medication, implantation of a pacemaker, or electrophysiological procedures. Determining the optimal treatment plan requires a comprehensive approach, including assessment of cardiac function, the degree of block, and the risk profile for each specific patient.
Experts also emphasize the significance of continuous monitoring of patients with atrioventricular block to promptly detect deterioration or potential complications. Modern treatment methods and the extensive experience of specialists allow for significant improvements in the prognosis of patients with this pathology and help prevent the development of serious cardiovascular complications.

Methods for diagnosing Atrioventricular block
The diagnosis of Atrioventricular block usually includes various methods such as electrocardiography (ECG) and Holter monitoring, which allow for the assessment of the heart’s electrical activity and the identification of conduction disturbances. Electrophysiological study of the heart (EPS) may be conducted for a more detailed evaluation of the heart’s conduction system, especially in cases of complex forms of atrioventricular block. Additional diagnostic methods may include cardiac magnetic resonance imaging (MRI) or echocardiography to assess the structure and function of the heart.
When diagnosing Atrioventricular block, it is also important to consider the clinical manifestations and medical history of the patient, which helps doctors determine the type and degree of the block, as well as possible causes of its occurrence. A comprehensive approach to diagnosis, based on medical knowledge and the use of modern equipment, allows for a more accurate determination of the state of the cardiac conduction system and the development of an individualized treatment plan for each patient.
- Electrocardiography (ECG): The primary diagnostic method that records the electrical activity of the heart, allowing the evaluation of possible conduction disturbances.
- Holter monitoring: A method that allows continuous monitoring of the patient’s heart activity over a specified period of time.
- Electrophysiological study of the heart (EPS): An invasive method that allows a more detailed study of the electrical activity of the heart and the identification of hidden disturbances.
- Magnetic resonance imaging (MRI) of the heart: A non-invasive method that allows for the evaluation of the structure and function of the heart, as well as the identification of possible pathologies.
- echocardiography: An ultrasound method used for visualizing and assessing the heart’s structure and function, including the examination of conduction systems.
Approaches to the treatment of Atrioventricular block
Treatment of atrioventricular block may include the use of antiarrhythmic medications, the implantation of a cardiac pacemaker, as well as the correction of any known causes of the block. It is important to individualize treatment in each specific case, considering factors that affect cardiac conductivity and function. Regular monitoring and follow-up are important to assess the effectiveness of the treatment and make any necessary adjustments.
- Use of a pacemaker: In cases of severe or symptomatic Atrioventricular block, implantation of an artificial heart driver, a pacemaker, is performed to maintain a normal heart rhythm.
- Use of antiarrhythmic medications: The doctor may prescribe antiarrhythmic drugs to control heart arrhythmias and improve heart conduction.
- Correction of the causes of the block: When the cause of the block is known, such as conduction disturbances due to ischemia, infarction, or toxic effects, it is necessary to correct the underlying disease to improve the condition of heart conduction.
- Medical treatment of the underlying disease: If the atrioventricular block is due to comorbid conditions, such as infectious or inflammatory processes, treatment may include the use of appropriate medications.
- Regular monitoring and adjustment of treatment: After establishing the diagnosis and starting treatment, it is important to conduct regular medical monitoring to assess the effectiveness of the prescribed treatment and make adjustments as needed.
Prevention measures of Atrioventricular block
In cases where a patient has already been diagnosed with atrioventricular block or is at high risk of its occurrence, a doctor may recommend a personalized prevention plan that includes the use of certain medications or the appointment of a pacemaker. Adhering to all of the doctor’s recommendations and regularly monitoring the condition of the cardiovascular system are key components of successful prevention of heart disorders, including atrioventricular block.
- Maintaining a healthy lifestyle, including regular physical exercises that contribute to strengthening the cardiovascular system.
- Adhering to a healthy diet rich in nutrients and low in saturated fats, with the aim of maintaining normal cholesterol levels and controlling blood pressure.
- Giving up harmful habits such as smoking and alcohol consumption, which reduces the risk of developing cardiovascular diseases.
- Regular medical check-ups and consultations to identify and monitor risk factors that could lead to the occurrence of atrioventricular block.
- An individualized prevention plan developed by a doctor based on the patient’s individual characteristics and taking into account risk factors associated with the development of atrioventricular block.
Amazing aspects of Atrioventricular block
Additionally, although atrioventricular block is typically associated with heart diseases and aging, it can also occur in children and infants with congenital heart abnormalities. This fact emphasizes the importance of early diagnosis and monitoring of heart health across all age groups. A comprehensive approach to understanding and treating atrioventricular block opens up interesting research directions aimed at improving the quality of life for patients with this condition.