Atrophic gastritis: common signs and effective treatment
- Understanding Atrophic Gastritis: Key Facts and Mechanisms
- Risk factors for atrophic gastritis
- The clinical picture of atrophic gastritis
- Expert opinion on strategies for treating atrophic gastritis
- Methods for diagnosing atrophic gastritis
- Strategies for treating atrophic gastritis
- Prevention measures for atrophic gastritis
- Interesting aspects of atrophic gastritis
- FAQ
Understanding Atrophic Gastritis: Key Facts and Mechanisms
Atrophic gastritis is a chronic inflammatory condition of the gastric mucosa characterized by the death of glandular cells and their replacement with connective tissue. This process leads to a disruption in the production of gastric juice, which can cause various disorders of the digestive system. The mechanism of development of atrophic gastritis is usually associated with Helicobacter infection, autoimmune processes, or chemical exposures such as alcohol consumption or certain medications.
It is important to note that atrophic gastritis can progress and become a risk factor for the development of certain diseases, including peptic ulcer disease, gastroesophageal reflux disease, and even stomach cancer. Understanding the key facts and mechanisms of this disease not only aids in early diagnosis and treatment but also helps in preventing complications and improving the quality of life for patients.
Risk factors for atrophic gastritis
The development of atrophic gastritis is due to a multifactorial etiology. The main risk factors include Helicobacter pylori infection, prolonged use of certain medications, autoimmune disorders, and genetic predispositions. Studies also link this type of gastritis to certain occupational risks, harmful habits, congenital gastrointestinal tract anomalies, as well as nutritional and psychological factors. A deep understanding of these factors is important for the prevention and effective treatment of atrophic gastritis.
- Helicobacter pylori infection: the most common cause of atrophic gastritis, infection may contribute to its development.
- Long-term use of NSAIDs: prolonged intake of medications such as aspirin or ibuprofen may increase the risk of developing atrophic gastritis.
- Autoimmune disorders: autoimmune atrophic gastritis develops due to the immune system attacking its own stomach wall cells.
- Genetic factors: the presence of certain genetic variants may increase susceptibility to the development of atrophic gastritis.
- Psychological factors: stress, depression, and other psychological issues can affect stomach function and contribute to the development of gastritis.
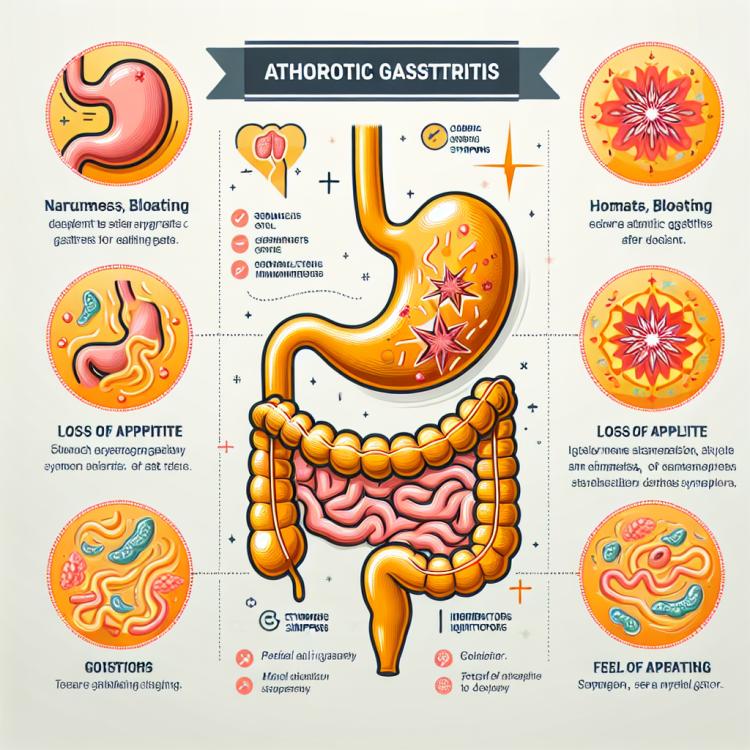
The clinical picture of atrophic gastritis
The clinical picture of atrophic gastritis may include various symptoms such as dyspepsia, nausea, belching, a feeling of fullness in the abdomen, appetite changes, vomiting, and pain or discomfort in the epigastric region. Patients may also experience weight loss, anemia, increased fatigue, and weakness. Additionally, the possible development of reflux esophagitis, peptic ulcer disease of the stomach and duodenum, as well as even precancerous conditions, is characteristic.
The diagnosis of atrophic gastritis can be conducted using gastroscopy with biopsy material for histological examination. Furthermore, laboratory tests may include the study of serum markers such as pepsinogen I and II, antibodies to Helicobacter pylori, as well as a complete blood count to detect concomitant anemia or inflammation. Understanding the nature of symptoms and proper diagnosis of atrophic gastritis play a key role in prescribing adequate treatment and preventing possible complications.
- Dyspepsia: Common symptoms of atrophic gastritis include digestive disturbances, such as a feeling of heaviness in the epigastrium and belching after meals.
- Appetite: Patients may experience a loss of appetite, leading to reduced food intake and, as a consequence, weight loss.
- Anemia: Due to impaired absorption of vitamins and minerals, atrophic gastritis can lead to the development of anemia.
- Reflux esophagitis: Patients often encounter excessive gastric contents spilling into the esophagus, causing reflux esophagitis.
- Fatigue and weakness: Chronic ailments associated with atrophic gastritis may lead to increased fatigue and weakness in patients.
Expert opinion on strategies for treating atrophic gastritis
Experts in gastroenterology recommend a comprehensive approach to the treatment of atrophic gastritis, which includes addressing the causes (for example, eradicating Helicobacter pylori in the presence of infection), maintaining gastrointestinal function, and preventing possible complications, including the development of precancerous changes. To reduce symptoms and improve the quality of life for patients, individualized pharmacotherapy regimens are often used, including contraceptive medications, probiotics, anti-secretory therapy, or anti-inflammatory drugs.
However, in light of the individuality of each clinical case, experts emphasize the importance of consulting with a physician and developing a personalized treatment plan for atrophic gastritis. Utilizing modern diagnostic and treatment methods based on the latest medical advancements will help achieve success in controlling this disease and prevent its progression.

Methods for diagnosing atrophic gastritis
The diagnosis of atrophic gastritis usually includes a clinical examination of the patient with an assessment of their medical history. However, the main diagnostic method is gastroscopy with biopsy sampling for histological examination. This method allows visualizing the condition of the mucous membrane, assessing the presence of inflammatory changes, and determining the degree of atrophy of the gastric secretory cells. In addition, laboratory studies, such as the examination of serum markers and blood tests, can complement the diagnostic process to obtain a more complete picture of the patient’s condition with atrophic gastritis.
- Gastrointestinal endoscopy: the primary method for visualizing the condition of the mucous membrane, determining inflammatory changes, and the degree of atrophy.
- Biopsy sampling: allows for histological examination to confirm the diagnosis of atrophic gastritis.
- Laboratory tests: examination of serum marker levels, blood tests (e.g., complete blood count, level of pepsinogen, and antibodies to Helicobacter pylori).
- X-ray of the stomach: may sometimes be used for additional assessment of the gastrointestinal tract’s condition.
- Repeat examinations and monitoring: it is necessary to conduct follow-up studies to assess the effectiveness of treatment and the patient’s condition over time.
Strategies for treating atrophic gastritis
- Elimination of Helicobacter pylori: In case of detection of Helicobacter pylori infection, eradication therapy aimed at destroying this bacterium is recommended.
- Acid-reducing medications: The doctor may prescribe medications that reduce acid production in the stomach to alleviate symptoms and reduce irritation of the mucous membrane.
- Medications for protecting and restoring the mucous membrane: To strengthen the mucous membrane and stimulate the healing of ulcers, medications that promote rapid tissue recovery may be prescribed.
- Probiotics and digestive enhancement medications: Probiotics help restore the normal intestinal microflora, while digestive enhancement medications aid in better absorption of food.
- Rational nutrition and maintaining a healthy lifestyle: An important part of treatment is following a diet, avoiding irritating foods, consuming easily digestible food, and maintaining a healthy lifestyle, including physical activity and quitting bad habits.
Prevention measures for atrophic gastritis
- Avoiding the use of aggressive medications: it is important to take only the medications prescribed by a doctor and to avoid self-medication, especially with drugs that can harm the gastric mucosa.
- Giving up bad habits: smoking and excessive alcohol consumption are risk factors for the development of atrophic gastritis. Completely quitting these habits can help prevent the disease.
- Healthy eating: it is advisable to consume food rich in vitamins and minerals, as well as to include probiotics in the diet to maintain a healthy gut microbiota, which can help prevent atrophic gastritis.
- Following a diet schedule: regular meals without snacks, moderate portions, and avoiding overeating contribute to the normal functioning of the gastrointestinal tract and can aid in the prevention of gastritis.
- Regular medical check-ups: it is important to regularly visit a doctor for preventive examinations, which will allow for the early detection of possible changes in the gastrointestinal tract and timely initiation of treatment.
Interesting aspects of atrophic gastritis
Another interesting aspect of atrophic gastritis is its connection with autoimmune disorders, where the body’s immune system turns against the cells of its own stomach. This feature of the disease requires additional attention when choosing appropriate treatment methods and monitoring the patient’s condition. All of this makes atrophic gastritis a subject of interest for researchers and practicing doctors focused on finding effective strategies for diagnosis and treatment.