Autoimmune hepatitis: symptoms, causes, and treatment
- Definition and essence of Autoimmune hepatitis
- Factors contributing to the development of autoimmune hepatitis
- Recognition of the symptoms of Autoimmune Hepatitis
- Expert opinion on the treatment of Autoimmune Hepatitis
- Current methods for diagnosing Autoimmune Hepatitis
- Effective methods for treating Autoimmune Hepatitis
- Measures for the prevention of Autoimmune Hepatitis
- Amazing aspects of autoimmune hepatitis disease
- FAQ
Definition and essence of Autoimmune hepatitis
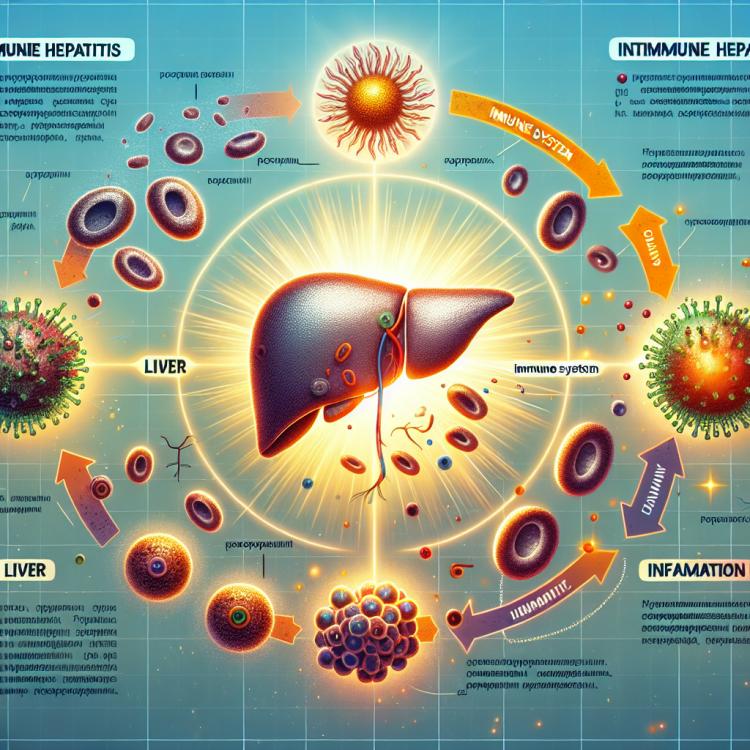
Autoimmune hepatitis is a chronic inflammatory liver disease caused by the body’s autoimmune response, where the immune system mistakenly attacks healthy liver cells. This leads to a gradual destruction of the liver and disruption of its functions. The main mechanisms underlying this disease are associated with disorders in the immune system, such as autoimmune antibodies, autoimmune lymphocytes, and cytokines that contribute to liver inflammation.
Factors contributing to the development of autoimmune hepatitis
Autoimmune hepatitis is the result of a malfunctioning immune system, wherein it begins to attack the liver’s own cells. The causes of this disease are not fully understood; however, it is believed that genetic predisposition may play a role. Additionally, external factors such as viral infections or environmental elements may be involved in the development of autoimmune hepatitis, which can trigger an autoimmune response.
Research also indicates a possible influence of hormonal changes on the development of autoimmune hepatitis, especially in women. Some medications may also contribute to the onset of immune attacks on the liver. Thus, the mechanism of autoimmune hepatitis onset is complex and multifaceted, necessitating further research for a complete understanding of its causes.
- Genetic predisposition: The presence of certain genetic factors may increase the likelihood of developing autoimmune hepatitis.
- Viral infections: Some viruses, such as hepatitis A, B, or C, may play a role in triggering the autoimmune response of the liver.
- Environment: Exposure to toxins, chemicals, or other harmful substances can disrupt immune system functions and contribute to the development of autoimmune hepatitis.
- Hormonal changes: In women, hormonal fluctuations, especially during pregnancy or menstruation, can affect immune system function and provoke the development of autoimmune hepatitis.
- Medications: Some medications, including antibiotics, anti-inflammatory drugs, and heart medications, can trigger an immune system reaction and contribute to the development of autoimmune hepatitis.
Recognition of the symptoms of Autoimmune Hepatitis
Autoimmune hepatitis can manifest with a variety of symptoms, including fatigue, pain in the right upper quadrant of the abdomen, jaundice, skin itching, and loss of appetite and weight. Some patients may experience symptoms characteristic of autoimmune diseases, such as joint pain, skin rashes, and increased fatigue.
The diagnosis of autoimmune hepatitis can be complex due to its diverse symptoms, which can overlap with other conditions. Accurate recognition of symptoms and their analysis in conjunction with the results of laboratory and instrumental studies help doctors make the correct diagnosis and initiate appropriate treatment.
- Fatigue and weakness: a constant feeling of fatigue can be one of the first signs associated with autoimmune hepatitis.
- Pain in the right upper quadrant of the abdomen: discomfort and pain in the area of the right hypochondrium may indicate liver problems.
- Jaundice: yellowing of the skin and the sclerae of the eyes, as well as dark urine pigment, are classic signs of liver damage.
- Skin itching: persistent skin itching without visible causes may be related to liver dysfunctions characteristic of autoimmune hepatitis.
- Loss of appetite and weight: decreased appetite, as well as unintentional weight loss, can be signs of liver dysfunction, including autoimmune hepatitis.
Expert opinion on the treatment of Autoimmune Hepatitis
Experts in the field of hepatology recommend a comprehensive approach to the treatment of Autoimmune Hepatitis. The primary goal of therapy is to suppress the immune system to reduce inflammatory processes in the liver. For this, glucocorticoids such as prednisolone, as well as immunomodulators like azathioprine, are often used.
Experts also note that early detection and treatment of Autoimmune Hepatitis play an important role in the prognosis of the disease. An individualized approach to the patient, regular monitoring of their condition, and adjustment of therapy under the supervision of a specialist contribute to the effective management of this serious liver disease.

Current methods for diagnosing Autoimmune Hepatitis
For the diagnosis of Autoimmune Hepatitis, various methods are widely used, including clinical studies, laboratory tests, and instrumental procedures. Clinical signs of the disease can be identified during the patient’s examination, including the analysis of symptoms, complaints, and previous medical history. Laboratory tests, such as blood tests, including liver function indicators and specific antibodies, are an important part of the diagnosis of Autoimmune Hepatitis.
Instrumental diagnostic methods, such as ultrasound examination, computed tomography, and magnetic resonance cholangiography, can help detect changes in the liver and bile ducts. To confirm the diagnosis, a liver biopsy is sometimes required, which allows for the assessment of the degree of inflammation and fibrosis, as well as the identification of characteristic changes typical of Autoimmune Hepatitis.
- Clinical examination: the doctor analyzes symptoms, patient complaints, and medical history to identify clinical signs of the disease.
- Laboratory tests: include blood tests for liver function indicators, such as levels of aminotransferases and bilirubin, as well as specific antibodies crucial for diagnosing Autoimmune hepatitis.
- Ultrasound examination: allows assessment of the liver and biliary tract condition, as well as detection of possible changes related to the disease.
- Computed tomography: is used for more detailed visualization of the liver and other abdominal organs to detect changes typical of Autoimmune hepatitis.
- Magnetic resonance cholangiography: allows examination of the biliary tract and determination of its condition in the context of liver diseases, including Autoimmune hepatitis.
Effective methods for treating Autoimmune Hepatitis
In cases where treatment with immunosuppressants is not sufficiently effective, or when side effects occur, more aggressive therapy may be required, including the use of other immunosuppressive agents or even liver transplantation. The optimal treatment strategy is chosen individually, taking into account the patient’s characteristics, the severity of the disease, and the presence of complications.
- Immunosuppressants: The use of azathioprine and prednisone to reduce the activity of the immune system.
- Combination therapy: The use of several drugs in combination for effective disease control.
- Monitoring condition: Regular observation of the patient to assess treatment effectiveness and prevent complications.
- Alternative immunosuppressive drugs: The use of other agents to suppress the immune response when primary drugs are insufficiently effective.
- Liver transplantation: In extreme cases, when other methods are ineffective, liver transplantation may be required to save the patient’s life.
Measures for the prevention of Autoimmune Hepatitis
It is also important to regularly undergo medical examinations and consultations with a doctor, especially in the presence of a hereditary predisposition to autoimmune diseases or other liver diseases. Timely detection and treatment of liver pathologies can help prevent the development of severe forms of diseases, including Autoimmune Hepatitis.
- Avoid harmful habits: quitting alcohol and smoking reduces the risk of developing liver pathologies, including Autoimmune hepatitis.
- Maintain a healthy lifestyle: regular physical activity, balanced nutrition, and moderate weight contribute to overall immune strengthening.
- Avoid contact with pesticides: prevent possible exposure to toxic substances that can negatively affect liver function.
- Undergo regular medical examinations: timely detection of liver pathologies helps prevent the development of severe forms of diseases, including Autoimmune hepatitis.
- Consult with a doctor if necessary: if there is a hereditary predisposition or other risk factors, be sure to discuss preventive measures with a medical professional.
Amazing aspects of autoimmune hepatitis disease
Another interesting point is the difference in clinical manifestations of autoimmune hepatitis across different age groups. For example, in children, the disease often presents as an acute form of symptoms, while in adults, a chronic nature and slower progression may prevail. Studying such aspects allows for a better understanding of the pathogenesis of the disease and the development of more effective methods for diagnosis and treatment.