Balanoposthitis: features of diagnosis and treatment methods
- Fundamentals of balanoposthitis: understanding symptoms, causes, and treatment
- Etiology of balanoposthitis
- The clinical picture of balanoposthitis
- Expert opinion on the treatment of balanoposthitis
- Methods for diagnosing balanoposthitis
- Methods of treating balanoposthitis
- Preventive measures for balanoposthitis
- Unexplained facts about balanoposthitis
- FAQ
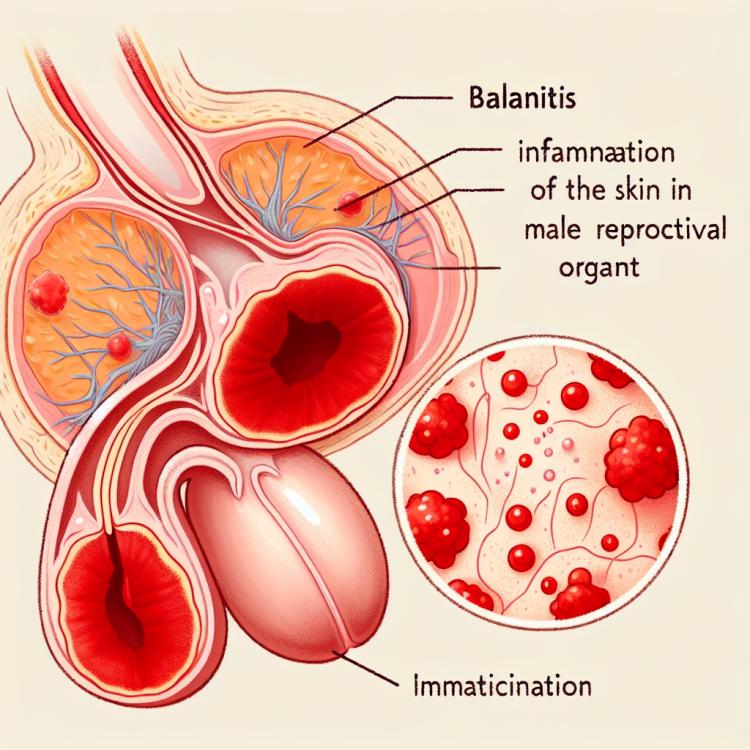
Fundamentals of balanoposthitis: understanding symptoms, causes, and treatment
Balanoposthitis is an inflammatory disease affecting the glans of the penis. Symptoms of balanoposthitis may include redness, swelling, itching, burning, discharge, and tenderness in the area of the glans. The origin of balanoposthitis is associated with infectious agents, irritants, allergic reactions, as well as improper care of the genital organs. Treatment of balanoposthitis includes hygiene measures, the use of local anti-inflammatory agents, antibiotics in the case of an infectious nature of the disease, as well as the elimination and prevention of the underlying causes of the disease.
Etiology of balanoposthitis
Balanoposthitis can have a variety of etiological factors, including infections, allergic reactions, trauma, inadequate hygiene, as well as genetic and immune factors. Infectious agents, such as bacteria, viruses, fungi, and yeast-like fungi, may be the primary cause of developing balanoposthitis. Some of them are capable of causing inflammatory processes on the skin of the genital organs, which can lead to the development of balanoposthitis.
In addition, allergic reactions to certain chemicals used in cleaning agents or lubricants can also be a cause of balanoposthitis. Damage to the skin in the genital area, for example, from trauma or friction, can create favorable conditions for the development of inflammatory processes and, consequently, balanoposthitis.
- Infections: Balanoposthitis is often caused by infectious agents such as bacteria, viruses, fungi, and yeast-like fungi.
- Allergic reactions: Reactions to chemicals used in cleaning agents or lubricants can contribute to the development of balanoposthitis.
- Injuries: Damage to the skin in the genital area, such as from rubbing or injury, can create conditions for the development of inflammation.
- Inadequate hygiene: Insufficient hygiene of the genital area can promote the development of inflammatory processes and balanoposthitis.
- Genetic factors: Some genetic characteristics may influence individual susceptibility to the development of balanoposthitis.
The clinical picture of balanoposthitis
Symptoms of balanoposthitis may include redness, swelling, itching, tingling, and pain in the area of the glans penis. Patients may also experience irritation and discharge from the urethra. Depending on the specific pathogen, the causes, and the degree of inflammation, symptoms can vary, and the diagnosis should be based on objective examination and history.
In some cases, balanoposthitis may present with more severe symptoms, such as the formation of ulcers and sores, purulent discharge, elevated body temperature, swelling of tissues, and even disturbances in urination. If such symptoms occur, it is important to consult a doctor for professional advice and appropriate treatment.
- Redness and swelling: the affected area may become red and swollen due to inflammation.
- Itching and discomfort: patients may experience itching and unpleasant sensations in the area of the glans penis.
- Painful urination: balanoposthitis may cause pain or discomfort during urination.
- Discharge and tingling: some patients may notice discharge from the urethra and feel tingling.
- Odor and irritation: balanoposthitis may be accompanied by an unpleasant odor, as well as irritation of the skin in the genital area.
Expert opinion on the treatment of balanoposthitis
Expert opinions on the treatment of balanoposthitis reflect the need for an individual approach to each patient. Doctors usually advise starting treatment with identifying the cause of the disease, as identifying the underlying pathogen is key to effective therapy. Standard treatment often includes a combination of antibiotics, antifungal agents, or anti-inflammatory drugs, depending on the type of infection and circumstances.
Experts also emphasize the importance of maintaining proper hygiene and precautions to avoid the recurrence of balanoposthitis. Regular check-ups and visits to the doctor can help monitor the healing process and prevent complications. Expert opinions on the treatment of balanoposthitis highlight the need for a comprehensive approach aimed at addressing the causes, symptoms, and preventing recurrences of this condition.

Methods for diagnosing balanoposthitis
The diagnosis of balanoposthitis includes a thorough clinical examination of the glans penis area, as well as taking a medical history considering possible infections, allergic reactions, and other factors that could cause an inflammatory response. Laboratory tests may be required to confirm the diagnosis, such as scraping analysis from lesions on the glans to identify pathogens, conducting a bacteriological examination of discharge, as well as dermatological examination.
If necessary, the doctor may prescribe additional diagnostic methods, such as culture studies, PCR diagnostics, skin allergy tests, or biopsy to establish the detailed nature of the inflammatory process. Timely detection and accurate determination of the causes of balanoposthitis are important in order to choose the most effective and individualized treatment method.
- Clinical examination by a doctor to assess the condition of the skin and mucous membranes of the genitals.
- Analysis of the patient’s history to identify risk factors such as infections or allergic reactions.
- Laboratory examination of scrapings from lesions on the skin of the glans penis to identify pathogens.
- Bacteriological study to determine the type of microorganism causing the inflammation.
- Dermatological examination to clarify the nature of the inflammatory process on the skin of the genitals.
Methods of treating balanoposthitis
In more serious cases of balanoposthitis, when there are complications or recurrences, surgical intervention may be necessary. Surgical treatment methods may include draining an abscess, removing affected tissues, or correcting anomalies that contribute to the development of the inflammatory process. Using a comprehensive approach to treating balanoposthitis, taking into account the individual characteristics of the patient and the causes of the disease, allows for the best results and helps prevent possible complications.
- Antibiotic therapy: the use of antibiotics to combat the infectious agent that caused balanoposthitis.
- Topical preparations: the use of local anti-inflammatory agents to relieve symptoms and reduce inflammation at the site of the lesion.
- Hygienic procedures: adhering to rules of hygiene for the genital organs to prevent recurrences and reduce the risk of infection.
- Surgical intervention: in cases of complications or ineffectiveness of conservative treatment, surgical treatment may be required to address problematic areas.
- Avoiding possible allergens: identifying and eliminating allergens that contribute to the occurrence of balanoposthitis, to prevent new cases of the disease.
Preventive measures for balanoposthitis
It is also important to monitor the state of the immune system, eliminate chronic diseases, lead a healthy lifestyle, and give up bad habits. Visiting a doctor at the first signs of inflammation, timely diagnosis, and treatment of other diseases that contribute to the development of balanoposthitis will help prevent its occurrence.
- Hygiene compliance: Regular and gentle cleaning of the head of the penis without the use of harsh cleaning agents.
- Injury prevention: Avoiding mechanical injuries to the genitals, securely wearing protective underwear during sports activities.
- Avoiding contact with irritating substances: Preventing the possible development of an inflammatory reaction by avoiding contact with aggressive chemicals.
- Maintaining a healthy lifestyle: Regular physical exercise, a balanced diet, and refraining from harmful habits can strengthen immunity and reduce the risk of balanoposthitis.
- Timely visit to a doctor: If the first signs of inflammation appear, it is necessary to promptly consult a specialist to prevent serious complications and ensure proper treatment.
Unexplained facts about balanoposthitis
Another interesting fact about balanoposthitis is its diverse symptoms and various treatment approaches, which can complicate diagnosis and the selection of the optimal therapy method. In addition, there is ambiguity in the area of disease prevention, as the effectiveness of different measures to prevent balanoposthitis can vary depending on the individual factors of each patient.