Bile reflux gastritis: symptoms, diagnosis, and effective treatment
- Definition of biliary reflux gastritis
- Etiology of biliary reflux gastritis
- The clinical picture of biliary reflux gastritis
- The specialists’ view on the therapy of biliary reflux gastritis
- Methods for diagnosing biliary reflux gastritis
- Methods of therapy for biliary reflux gastritis
- Prevention measures for biliary reflux gastritis
- Interesting aspects of biliary reflux gastritis
- FAQ
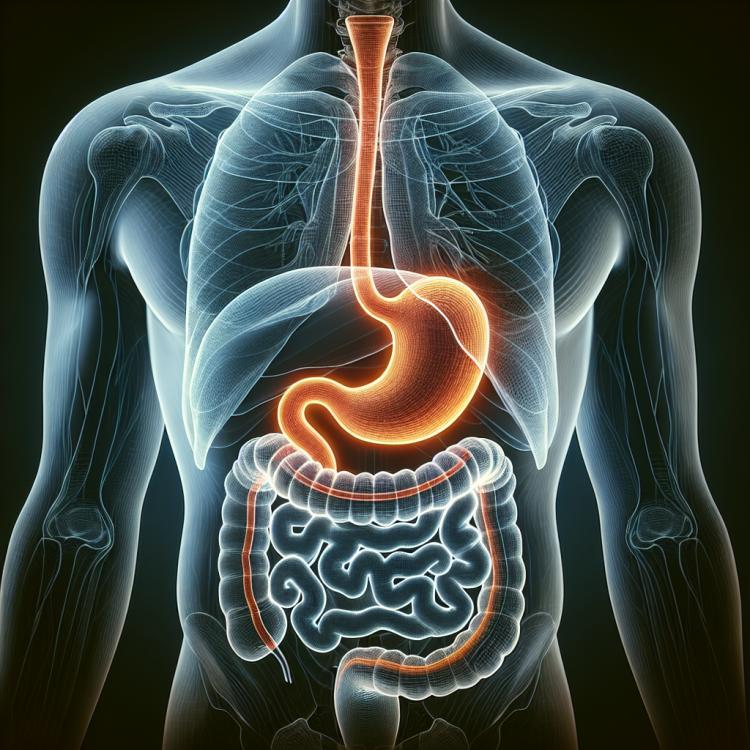
Definition of biliary reflux gastritis
Biliary reflux gastritis is an inflammatory disease of the gastric mucosa, caused by the backflow of bile from the duodenal part of the duodenum into the stomach. This process occurs due to dysfunction of the sphincter that separates the bile duct and the common duct of the stomach. Biliary reflux gastritis is often accompanied by symptoms of dyspeptic syndrome, such as heartburn, belching, nausea, and discomfort in the epigastric region. Additionally, this disease can provoke the development of gastroduodenal pathology and requires a differentiated diagnostic approach for the optimal treatment.
Etiology of biliary reflux gastritis
Biliary reflux gastritis is usually caused by the regurgitation of bile from the duodenum into the stomach. This process is accompanied by the destruction of the gastric mucosa and causes inflammatory changes. The most common causes of biliary reflux gastritis are dysfunction of the Oddi sphincter, gallstones, and other gastrointestinal disorders that create a blockage in the normal flow of bile. These factors can lead to prolonged and increased pressure in the bile duct, causing bile reflux and the development of gastritis.
- Oddi sphincter dysfunction: Disorders of the Oddi sphincter can lead to improper closure of the bile duct, promoting the regurgitation of bile into the stomach.
- Gallstone: The presence of gallstones, especially in the area of the bile duct or gallbladder, can be one of the causes of biliary reflux gastritis.
- Movement of intestinal gases: Uncontrolled movements of gas through the esophagus can cause pressure changes in the stomach, promoting bile reflux.
- Peristalsis disorder: Weakening of the gastrointestinal tract muscles or disruption of intestinal movement coordination can lead to improper movement of food and fluids, including bile, causing reflux and irritation of the stomach lining.
- Bile duct pathology: Any abnormalities in the anatomy or function of the bile duct, such as narrowing, tumors, or inflammation, can contribute to the development of biliary reflux gastritis.
The clinical picture of biliary reflux gastritis
The clinical picture of biliary reflux gastritis is characterized by a wide range of symptoms, including dyspeptic manifestations such as nausea, vomiting, discomfort in the epigastric region, belching, and a feeling of fullness in the stomach after eating. Patients also often complain of heartburn, belching with a bitter taste, and a feeling of bitterness in the mouth, which may be associated with bile reflux into the esophagus from the stomach. In some cases, biliary reflux gastritis can lead to the development of peptic ulcer disease of the stomach and duodenum, as well as cause gastro-duodenal reflux disease.
- Dyspeptic manifestations: dyspeptic symptoms of biliary reflux gastritis include nausea, vomiting, discomfort in the epigastric area, belching, and a feeling of fullness in the stomach after eating.
- Heartburn: patients may experience a burning sensation behind the sternum, which is associated with the reflux of bile and food acids from the stomach into the esophagus.
- Bitter belching: a feeling of bitterness in the mouth and the appearance of a bitter taste may be related to bile reflux.
- Peptic ulcer disease: in some cases, biliary reflux gastritis may contribute to the development of ulcers in the stomach and duodenum.
- Gastro-duodenal reflux disease: biliary reflux gastritis can lead to the development of gastro-duodenal reflux disease, resulting in a chronic inflammatory process in the stomach and duodenum.
The specialists’ view on the therapy of biliary reflux gastritis
Experts emphasize the importance of a comprehensive approach to the therapy of bile reflux gastritis, which may include pharmacological treatment, diet, and lifestyle changes. It is worth noting that effective management of this condition may involve the use of medications to reduce gastric acidity as well as agents that help relieve symptoms. Some experts also recommend paying attention to medications that facilitate the normalization of stomach contractions and the movement of food through the gastrointestinal tract to prevent recurrences.
Equally important, in the opinion of specialists, is rational dietary therapy aimed at reducing the burden on the gastrointestinal tract and lowering the risk of exacerbations. Limiting the intake of fatty and spicy foods, consuming food in small portions, and avoiding eating before bedtime may contribute to improving the condition of patients with bile reflux gastritis.

Methods for diagnosing biliary reflux gastritis
Diagnosis of biliary reflux gastritis usually involves a comprehensive approach that includes clinical assessment of symptoms, results of physical examination, and laboratory studies such as blood tests for markers of inflammation and liver function. Accurate diagnosis often requires instrumental and functional studies, such as esophagogastroscopy with biopsy, ultrasound of the abdominal organs, cholecystocystography, or magnetic resonance cholangiography.
- Esophagogastroscopy with biopsy: this study helps assess the condition of the mucous membrane of the esophagus and stomach, as well as to take tissue samples for further analysis.
- Ultrasound examination of the abdominal organs: allows assessment of the structure and function of the bile ducts and digestive organs, identifying the presence of stones and other pathologies.
- Cholecystocystography: this method of investigation allows evaluation of the function of the gallbladder and determination of possible disorders in the bile excretion process.
- Magnetic resonance cholangiography: an innovative method used for visualizing bile ducts and identifying possible pathologies without the use of X-ray radiation.
- Tests of blood and urine: test results can reflect the level of inflammation, liver function, and other indicators, aiding in the diagnosis of biliary reflux gastritis.
Methods of therapy for biliary reflux gastritis
In some cases, surgical intervention is required to restore the functionality of the stomach and esophagus, especially in the presence of ulcerative lesions or strictures. Surgical methods, such as fundoplication or restoration of the gastrointestinal tract, may be used as an effective way to combat biliary reflux gastritis.
- Pharmacotherapy: The treatment of bile reflux gastritis may include the use of medications to reduce stomach acidity, antacids, prokinetics to improve gastrointestinal motility, and agents to protect the mucous membrane.
- Diet: Regulating the diet may be an important part of the treatment, including the consumption of easily digestible and non-irritating foods, and limiting fatty, spicy, and acidic foods.
- Regular monitoring: Surgical interventions and changes in treatment may require regular monitoring by specialists to assess the effectiveness of therapy and adjust the action plan if necessary.
- Physical therapy: Physical exercises, massage, and other physical therapy methods may help improve digestion and the overall condition of the patient.
- Psychotherapy: Given the connection between pain symptoms and mental state, psychotherapy may be an important component of the comprehensive treatment of bile reflux gastritis.
Prevention measures for biliary reflux gastritis
It is important to pay attention to seeking medical advice promptly when characteristic symptoms appear, which will allow for diagnosis and the initiation of treatment at an early stage of the disease. Regular medical check-ups and adherence to doctor’s recommendations also contribute to the prevention of complications of bile reflux gastritis and the maintenance of the patient’s overall health.
- Adhering to a healthy diet: limiting the consumption of fatty, spicy, and fried foods, increasing the intake of vegetables, fruits, and whole grains.
- Giving up bad habits: quitting smoking and moderate alcohol consumption will help reduce the risk of developing biliary reflux gastritis.
- Regular physical activity: exercising contributes to the normalization of metabolism, improves the functioning of the digestive system, and prevents gastrointestinal diseases.
- Consuming enough water: maintaining hydration supports the normal functioning of the gastrointestinal tract.
- Regular check-ups with a doctor: timely medical attention when characteristic symptoms appear allows for necessary diagnostics and the initiation of treatment in the early stages of disease development.
Interesting aspects of biliary reflux gastritis
Another interesting fact is the possible progression of biliary reflux gastritis to more serious gastrointestinal pathologies, such as peptic ulcer disease or even stomach cancer. Therefore, it is important to seek medical help promptly when characteristic symptoms arise and to follow the doctor’s recommendations to prevent complications and ensure effective treatment.