Olle’s disease: symptoms, causes and treatment
- Understanding the origin and nature of Olier’s Disease
- Factors contributing to the development of Olier’s disease
- Main signs and symptoms of Olier’s disease
- Expert opinion on the treatment of Olier’s disease
- Methods for diagnosing Ollier’s disease
- The main methods of treatment for Olier’s disease
- Preventive measures for Olle’s Disease
- More about Olie’s Disease
- FAQ
Understanding the origin and nature of Olier’s Disease
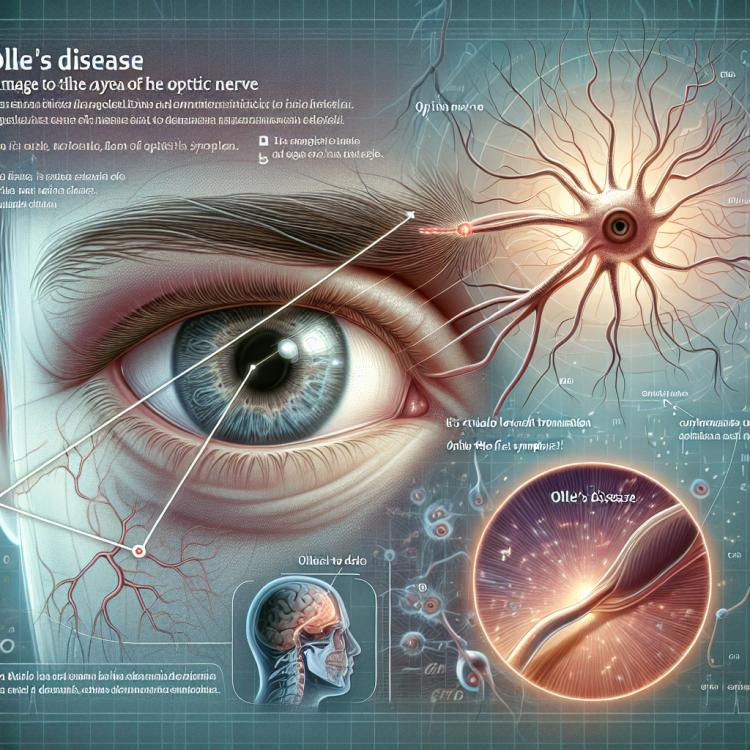
The Ollier disease, also known as neuromyelitis optica spectrum, is a rare inflammatory disease of the central nervous system, characterized by damage to the optic nerve and spinal cord. This pathology is caused by an autoimmune process, where the immune system targets the body’s own tissues, particularly the myelin sheaths of nerve fibers. Similar to other autoimmune diseases, the development mechanism of Ollier disease includes genetic, immunological, and environmental factors that may contribute to the activation of the immune system and the development of characteristic clinical manifestations.
To accurately understand the origin and nature of Ollier disease, further research aimed at identifying specific genetic mutations and immunological mechanisms underlying this condition is necessary. Such studies may help not only in improving the accuracy of diagnosis and prognosis of Ollier disease but also in developing new effective treatment and prevention methods for this condition.
Factors contributing to the development of Olier’s disease
Ollier’s disease, also known as optic neuritis, is often associated with immune-related processes, including autoimmune reactions of the body. Research indicates the important role of disturbances in the immune system in the onset of this disease. Factors contributing to the development of Ollier’s disease may also include genetic predispositions, viral infections, or other external influences that cause disruptions in the function of the optic nerve and lead to the characteristic symptoms of this disease.
- Autoimmune reactions: The immune system may mistakenly attack its own tissues, including the optic nerve, contributing to the development of Olie’s disease.
- Genetic predisposition: Hereditary factors can play an important role, increasing the likelihood of developing Olie’s disease.
- Viral infections: Some viruses can provoke immune reactions that contribute to the development of this disease.
- Environmental influences: Factors such as stress, exposure to toxic substances, or infections can have a negative impact on the state of the optic nerve.
- Immunosuppression: A decrease in the body’s protective functions may increase the susceptibility to various immune disorders, including Olie’s disease.
Main signs and symptoms of Olier’s disease
The Olie disease is most often characterized by a sudden onset of symptoms, including loss of vision, exacerbation or complete loss of visual functions, often developing over a period of days to weeks. Patients may also experience pain with eye movement, color vision disturbance, and photophobia. In addition, symptoms related to increased sensitivity of the eyeball may occur, such as tenderness and irritation.
Characteristic clinical signs of Olie disease include constriction of the visual fields, which can lead to the appearance of tunnel vision in patients. Other symptoms include disruptions in color perception, double vision, and changes in visual acuity. Patients may also experience problems with eye coordination when focusing and shifting gaze, which affects the overall quality of visual functions.
- Loss of vision: Ollier’s disease is often characterized by exacerbation or complete loss of visual functions.
- Pain with eye movement: Patients may experience discomfort and pain in the eyes when trying to move them.
- Color vision: Disturbances in color perception may be observed in people with Ollier’s disease.
- Photophobia: Increased sensitivity to bright light may be one of the symptoms of this condition.
- Narrowing of visual fields: Patients may experience narrowing of the visual field, which causes a tunnel effect.
Expert opinion on the treatment of Olier’s disease
When considering treatment methods for Olé disease, experts emphasize the importance of a comprehensive approach that includes the use of high-dose corticosteroids to reduce inflammation, immunomodulatory drugs to stabilize the immune system, and plasmapheresis to cleanse the blood of antibodies. The effectiveness of treatment often depends on the timely initiation of therapy and the combination of various methods depending on the stage and characteristics of the disease.
Experts also discuss the prospects of new treatment methods, such as the use of monoclonal antibodies or gene therapy techniques for a more targeted effect on the mechanisms of optic neuritis development. Individualizing the approach for each patient and finding the optimal combination of therapeutic measures are key aspects that experts focus on in the context of treating Olé disease.

Methods for diagnosing Ollier’s disease
Diagnosis of Olie’s Disease is most often based on clinical symptoms such as vision loss, changes in color perception, and pain during eye movement. Additional diagnostic methods may include neurological examination, studying visual fields using perimetry, as well as examination of the fundus for changes characteristic of this condition.
In addition to clinical signs, various educational diagnostic methods may be used for diagnosing Olie’s Disease, such as magnetic resonance imaging (MRI) of the brain and optical coherence tomography (OCT) for visualizing the structures of the fundus and further studying changes in the optic nerve. Accurate and timely diagnosis plays an important role in determining the treatment strategy and predicting outcomes for patients with Olie’s Disease.
- Clinical symptoms: Include loss of vision, changes in color perception, and pain when moving the eyes.
- Neurological examination: Examination of the nervous system may be conducted to identify symptoms related to Ollier’s disease.
- Perimetry: A method of studying the visual field that helps identify possible anomalies and defects in visual function.
- Fundus examination: Allows for the detection of structural changes characteristic of the disease and assessment of the condition of the optic nerve.
- Magnetic resonance imaging (MRI) of the brain: Allows visualization of brain structures and identification of possible changes associated with Ollier’s disease.
The main methods of treatment for Olier’s disease
- Use of corticosteroids: The main treatment method for Olie’s disease includes the use of corticosteroids to reduce inflammation and improve visual functions by decreasing immune reactions.
- Immunomodulatory therapy: Additional methods include the use of immunomodulators aimed at correcting autoimmune processes and regulating the patient’s immune system.
- Intravenous immunoglobulins: Intravenous immunoglobulins may be used as an additional treatment method for Olie’s disease to improve neurological status and suppress immune reactions.
- Surgical intervention: In cases where conservative methods do not yield the expected results, patients may be recommended surgical correction to stabilize their condition and preserve visual functions.
- Systemic treatment: Therapy may include systemic approaches, such as the use of antiviral medications or other methods aimed at suppressing potential toxic or infectious factors contributing to the development and progression of Olie’s disease.
Preventive measures for Olle’s Disease
It is important to undergo regular medical examinations designed to detect disturbances in the visual system and neurological symptoms. Consulting specialists at the first signs of the disease will allow for timely treatment to prevent possible complications. Educating patients about the critical importance of early detection and treatment of Olie’s Disease can also play a key role in prevention and the successful fight against this disease.
- Maintaining a healthy lifestyle: Includes regular physical exercise, balanced nutrition, avoiding bad habits, and maintaining a normal weight to strengthen the immune system.
- Regular medical check-ups: Allow timely detection of disorders in the visual system and neurological symptoms, which contributes to early diagnosis and treatment of the disease.
- Avoiding stress: Helps maintain normal immune system function, reduces the risk of inflammatory processes, and may contribute to the prevention of Olier’s Disease.
- Education and awareness: Supporting patients in understanding symptoms and the importance of timely medical consultation for the prevention and treatment of this disease.
- Proper daily routine and rest: Important for overall strengthening of the body, maintaining psycho-emotional balance, and reducing stress impacts on the immune system.
More about Olie’s Disease
An interesting aspect of Olie disease is its variability and unpredictability in the development of symptoms in patients. Some patients may experience a single episode of optic neuritis without subsequent relapses, while others may have a chronic course of the disease, causing persistent problems with visual function. Studying these features helps specialists better understand the nature and character of the disease, which may influence treatment approaches and prognosis for patients.