Raynaud’s disease: symptoms, causes, and treatment
- Definition and main characteristics of Raynaud’s disease
- Etiology of Raynaud’s Disease
- The clinical picture of Raynaud’s disease
- Expert opinion on the treatment of Raynaud’s disease
- Methods of diagnosis in Raynaud’s disease
- Methods of treating Raynaud’s disease
- Reynaud’s Disease Prevention
- Amazing Aspects of Raynaud’s Disease
- FAQ
Definition and main characteristics of Raynaud’s disease
Raynaud’s disease, or rheumatic fever, is a systemic inflammatory disease caused by the incomplete resolution of a streptococcal infection. It is characterized by connective tissue damage, an autoimmune component, and predominantly affects young people. The main symptoms include fever, polyarthritis, carditis, and chorea, as well as the development of rheumatic nodules, skin lesions, and other manifestations, most often affecting the heart and joints.
Etiology of Raynaud’s Disease
Raynaud’s disease is a systemic autoimmune condition characterized by inflammation of the joints, blood vessels, and connective tissues. The detailed mechanisms of the onset of the pathology are not fully understood; however, it is believed that the immune system of the body begins to attack its own tissues, leading to inflammation and damage to organs.
The main causes of Raynaud’s disease include genetic predisposition, environmental influences, infections, and hormonal changes. Some scientific studies also associate the onset of the disease with dysfunctions of the immune system and an imbalance in cytokine production. Proper treatment and control of the factors that contribute to the development of the disease play an important role in managing Raynaud’s disease.
- Genetic predisposition: Hereditary factors may play a role in the onset of Raynaud’s disease; studies show that people with certain genetic variants have an increased likelihood of developing the condition.
- Environmental factors: Environmental factors such as smoking, exposure to chemicals, or infections can contribute to the development of the disease.
- Infections: Certain types of infections, such as viral or bacterial, can stimulate the immune system and provoke an autoimmune response, which may lead to Raynaud’s disease.
- Hormonal changes: Hormonal imbalances, especially in women, can affect the functioning of the immune system and contribute to the development of autoimmune diseases, including Raynaud’s disease.
- Cytokine imbalance: Some studies indicate the significance of changes in cytokine production, substances that regulate inflammatory processes and immune responses, in the onset and development of Raynaud’s disease.
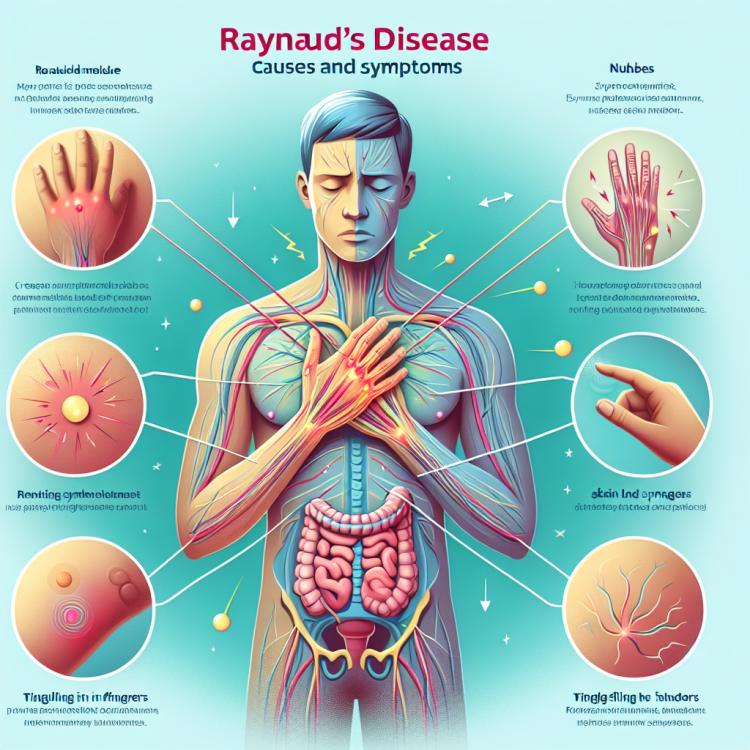
The clinical picture of Raynaud’s disease
The clinical picture of Raynaud’s disease can manifest a variety of symptoms, including characteristic pain and swelling in the joints, inflammation of blood vessels, skin manifestations, fatigue, and general malaise. Morning stiffness in the joints and elevated body temperature are often observed. Some patients may experience heart problems, including inflammation of the heart lining.
In addition, patients with Raynaud’s disease often face digestive disorders, weight loss, neurological symptoms, and depression. The range of symptoms can vary from mild to severe cases, and sometimes the disease can affect several systems of the body simultaneously. Understanding the clinical picture of Raynaud’s disease is an important aspect of diagnosing and treating this condition.
- Joint manifestations: pain, swelling, and morning stiffness in the joints are typical symptoms of Raynaud’s Disease.
- Inflammation of blood vessels: the disease can lead to inflammation of the vessels, which manifests on the skin as a rash or nodules.
- Fatigue and general malaise: patients often complain of a constant feeling of fatigue, even with minor physical exertion.
- Cardiac manifestations: inflammation of the heart may present as chest pain, arrhythmia, and a deterioration of general condition.
- Neurological symptoms and psychological disorders: some patients with Raynaud’s Disease may experience problems with memory, concentration, as well as depression and anxiety.
Expert opinion on the treatment of Raynaud’s disease
Expert opinion on the management of Raynaud’s Disease is based on a comprehensive approach, including the use of anti-inflammatory drugs, immunomodulators, and in some cases, glucocorticosteroids. Effective treatment aims not only to relieve symptoms but also to slow disease progression and prevent possible complications.
Experts also emphasize the importance of regular patient monitoring, adjusting the treatment plan based on disease dynamics, and maintaining a healthy lifestyle. The primary focus is on an individualized approach to treatment, taking into account the characteristics of each patient and striving to achieve the best clinical outcomes in the management of Raynaud’s Disease.

Methods of diagnosis in Raynaud’s disease
In case of suspicion of Raynaud’s disease, it is important to conduct a comprehensive diagnosis, including clinical examination, blood and urine tests, as well as instrumental examination methods. The clinical examination allows for the identification of characteristic symptoms of the disease, such as joint changes, skin manifestations, and signs of inflammation. Blood tests, including a general analysis and biochemical indicators, may indicate the presence of an inflammatory process and other anomalies.
Instrumental diagnostic methods, such as joint X-rays, ultrasound examination, computed tomography, or magnetic resonance imaging, help clarify the condition of joints, organs, and tissues. Additionally, immunological studies are conducted to confirm the autoimmune nature of the disease. The comprehensive use of various diagnostic methods allows for an accurate assessment of the patient’s condition and the appointment of appropriate treatment.
- Clinical examination: An integral part of the diagnosis, it includes the assessment of the patient’s general condition, identification of characteristic symptoms and signs of the disease.
- Blood and urine tests: A complete blood count, biochemical indicators, and immunological tests help assess inflammatory processes and immunological disorders.
- X-ray of joints: The examination using X-ray allows for the identification of structural changes in the joints and assessing the degree of their damage.
- Ultrasound examination: This method can be used to assess the joints, soft tissues, blood vessels, and other structures.
- Magnetic resonance imaging (MRI): Provides detailed images of internal organs, joints, and tissues, highlighting changes associated with the disease.
Methods of treating Raynaud’s disease
In addition to drug therapy, physiotherapy, rehabilitation, as well as special exercises and diet may be included in the comprehensive treatment of Raynaud’s Disease. Physiotherapy helps strengthen muscles, improve joint mobility, and reduce inflammation, while diet can aid in weight control and enhance overall health. It is important to individualize the treatment approach for each patient, considering the specifics of their condition and the extent of the disease’s manifestation.
- Anti-inflammatory drugs: Treatment of Raynaud’s disease often involves the use of non-steroidal anti-inflammatory drugs to reduce inflammation in the joints and alleviate pain.
- Glucocorticoids: In some cases, glucocorticoids may be used for rapid symptom relief and to suppress inflammation.
- Immunosuppressants: Medications in this class help to suppress the activity of the immune system and prevent aggressive autoimmune reactions in Raynaud’s disease.
- Physical therapy: Physical therapy procedures, such as ultrasound therapy, massage, and electrical stimulation, help improve circulation, strengthen muscles and joints, and reduce inflammation.
- Diet and exercise: A balanced diet and regular physical activity contribute to maintaining health, controlling weight, and improving overall condition in Raynaud’s disease.
Reynaud’s Disease Prevention
Educating patients about mindful self-care and monitoring their health status in the early stages can be key in the prevention of Raynaud’s disease. Long-term adherence to the doctor’s recommendations and regular follow-up with specialists can help detect and address this condition in a timely manner, which contributes to reducing the severity of symptoms and improving the prognosis of the disease.
- Maintaining a healthy lifestyle: regular physical exercise, a balanced diet, and refraining from harmful habits contribute to the overall strengthening of the body and a reduced risk of developing diseases.
- Infection prevention: following hygiene rules, vaccinations, and avoiding contact with individuals suffering from infectious diseases help decrease the likelihood of inflammatory processes often accompanying illness.
- Regular medical examinations: timely visits to the doctor and regular medical check-ups help identify potential health issues at early stages and prevent their development.
- Learning self-care: conscious awareness of one’s health, regular self-monitoring, and control over one’s lifestyle assist patients in leading a healthy life and responding promptly to changes in their body.
- Following the doctor’s recommendations: consistently adhering to specialists’ recommendations, following the prescriptions of the attending physician, and maintaining the prescribed regimen will help minimize the risk of developing Raynaud’s disease.
Amazing Aspects of Raynaud’s Disease
Another interesting fact about this disease is its connection to genetic factors. Hereditary predisposition may play an important role in the development of Raynaud’s disease, although the definitive mechanisms of this interaction are still not fully understood. Advances in molecular genetics and research in immunology continue to provide new insights into the remarkable aspects of this disease.