Bronchitis: everything you need to know
Definition of bronchitis
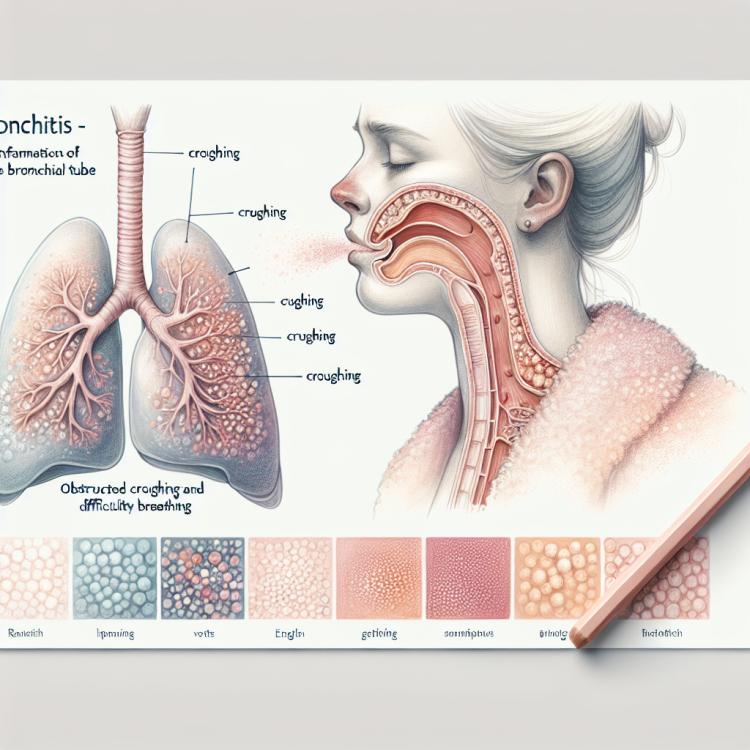
Bronchitis is an inflammation of the bronchial mucosa, characterized by cough and difficulty breathing. This condition can have both acute and chronic courses and is usually caused by viruses or bacteria. In bronchitis, there is often abundant mucus production, and there may be an increase in body temperature and general weakness.
Several forms of bronchitis are distinguished depending on severity, causes, and the nature of the disease course. Acute bronchitis usually lasts for several weeks and responds well to treatment, while chronic bronchitis may be accompanied by a deterioration in lung structure and require prolonged medical monitoring and treatment.
Factors contributing to the development of bronchitis
The development of bronchitis is usually due to various factors, including viral infections, smoking, environmental pollution, and genetic predispositions. Viruses, such as respiratory syncytial virus (RSV) and influenza, can cause inflammation of the bronchial tubes, leading to the development of bronchitis. Smoking is one of the main risk factors, as nicotine and other harmful substances found in tobacco smoke irritate the bronchial mucosa and promote inflammation.
Air pollution, contact with allergens or irritants, as well as prolonged exposure to high humidity or polluted conditions, can also contribute to the development of bronchitis. Genetic predispositions can also play a role in the occurrence of the disease, as some individuals may be more susceptible to inflammatory processes in the bronchial tubes due to hereditary factors.
- Viral infections: Respiratory syncytial virus (RSV) and influenza can cause inflammation of the bronchial tubes.
- Smoking: Nicotine and harmful substances in tobacco smoke irritate the bronchial mucosa, contributing to their inflammation.
- Environmental pollution: Contact with allergens or irritants, increased humidity, and air pollution can increase the risk of developing bronchitis.
- Genetic predispositions: Hereditary factors may play a role in increasing susceptibility to inflammatory processes in the bronchial tubes.
- Prolonged exposure to the lungs: Long-term exposure to irritants such as toxic gases or dust can contribute to the development of bronchitis.
Manifestations of bronchitis
Symptoms of bronchitis can vary depending on the type of disease and its severity. The main manifestations of bronchitis include coughing, often with phlegm production, which is a result of inflammation of the bronchial tubes and the body’s efforts to get rid of microorganisms or other irritants. The cough can be dry or productive, with the sputum potentially being clear, white, yellow, or green depending on the cause of inflammation.
In addition to coughing, patients with bronchitis often complain of difficulty breathing, shortness of breath, fatigue, and weakness. Some may experience chest pain or discomfort while breathing, which may also be related to inflammation of the bronchial tubes and accompanying processes in the lungs. In the case of acute bronchitis, symptoms may occur temporarily and improve over time; however, in the case of chronic bronchitis, symptoms may be persistent and require longer treatment.
- Cough: one of the main symptoms of bronchitis is a cough, which can be dry or accompanied by sputum production.
- Expectoration of sputum: patients with bronchitis may experience the expectoration of mucous-purulent or sputum of various colors.
- Shortness of breath: difficulty breathing, a feeling of pressure in the chest, and lack of air may be signs of bronchitis development.
- Fatigue and weakness: patients often report general tiredness, weakness, and malaise due to the body fighting the inflammatory process.
- Chest pain: some patients may feel discomfort, pressure, or pain in the chest as a result of the inflammation of the bronchial tubes.
Medical opinion on the treatment of bronchitis
Medical opinion on the management and treatment of bronchitis emphasizes the importance of an individualized approach for each patient, depending on the type of bronchitis, possible causes of the disease, and accompanying factors. Experts recommend seeking medical help at the first signs of illness, as early treatment contributes to more effective and rapid recovery. In most cases, symptomatic methods are used to treat acute bronchitis, such as taking cough suppressants to relieve coughing and ease breathing.
For chronic bronchitis, experts recommend a comprehensive approach that includes regular medical monitoring, lifestyle modifications (such as quitting smoking), physiotherapy procedures, the use of inhalation medications, and possibly antibiotics in the case of an infectious component. Effective treatment of bronchitis aims not only to alleviate symptoms but also to prevent exacerbations and maintain respiratory system functions over the long term.

Methods of diagnosing bronchitis
Diagnosis of bronchitis usually includes medical history collection, physical examination, as well as laboratory and instrumental methods of investigation. The doctor listens to the lungs with a stethoscope to detect characteristic sounds of breathing, wheezing, and whistling, which may indicate the presence of inflammation in the bronchial tubes. A clinical blood test, sputum analysis for the presence of infectious agents or other pathological processes can also help establish a diagnosis of bronchitis.
To more accurately determine the characteristics of the disease and rule out other possible causes of symptoms, additional diagnostics may be required, such as chest X-ray, computed tomography (CT), bronchoscopy, or functional breathing tests. These methods help establish the degree of inflammation, identify possible complications, and determine an appropriate treatment course for a patient with bronchitis.
- History taking: The doctor conducts a conversation with the patient to determine the nature of symptoms, duration of the disease, and presence of risk factors such as smoking or contact with infections.
- Physical examination: The doctor examines the patient, listens to the lungs with a stethoscope to identify wheezing, whistling, or other characteristic breathing sounds.
- Laboratory tests: A clinical blood test may reveal signs of inflammation, and a sputum analysis for bacteria or viruses helps identify the causative agent of the infection.
- Chest X-ray: Radiological examination allows for the assessment of lung condition and identification of changes associated with bronchitis.
- Pulmonary function tests: Used to assess lung volumes, airflow rates, and other parameters of breathing function.
Methods for treating bronchitis
In addition to medication therapy, it is recommended to maintain bed rest, consume an adequate amount of fluids, ventilate the room, and avoid exposure to irritants such as tobacco smoke or polluted air. In the case of chronic bronchitis, when the disease becomes recurrent, it is essential to follow the doctor’s recommendations, take medications regularly for an extended period, and undergo medical examinations to monitor lung condition and respiratory function.
- Drug therapy: Depending on the type of bronchitis and its cause, antibiotics, anti-inflammatory drugs, mucolytics, or bronchodilators may be used to alleviate symptoms and eliminate inflammation.
- Physiotherapy: Physiotherapy procedures, such as inhalations with medicinal preparations, help improve expectoration, relieve bronchospasms, and reduce swelling of the respiratory mucosa.
- Regimen and diet: It is important to adhere to bed rest during an exacerbation of bronchitis, drink plenty of warm fluids, and exclude from the diet foods that may enhance inflammation or cause allergic reactions.
- Avoiding irritants: It is important to eliminate exposure to irritants such as tobacco smoke, smoke from fires, and drafts, which can exacerbate bronchitis symptoms and slow down the recovery process.
- Herbal therapy: An additional method of treatment may be the use of herbal teas, decoctions, or tinctures that have mucolytic, anti-inflammatory, or general strengthening effects.
Prevention of bronchitis
Preventive vaccinations against viral diseases that can cause bronchitis, as well as adherence to hygiene measures, including regular hand washing and avoiding contact with individuals suffering from respiratory infections, help reduce the likelihood of illness. An important aspect of prevention is also timely treatment of other respiratory diseases to prevent their progression and the development of complications, including bronchitis.
- Avoid smoking: Active and passive smoking is one of the main risk factors for developing bronchitis.
- Maintain a healthy lifestyle: Regular physical exercise, healthy eating, and adequate rest will help strengthen the immune system and reduce the likelihood of bronchitis.
- Vaccination: Preventive vaccinations against viruses such as influenza can help prevent the development of bronchitis caused by viral infections.
- Hand hygiene: Regular hand washing and avoiding contact with individuals suffering from respiratory infections help prevent the transmission of pathogens.
- Strengthening immunity: Taking measures to strengthen the body, including consuming vitamins, minerals, and prebiotics, contributes to enhancing the body’s protective functions and reducing the risk of bronchitis.
Unusual aspects of bronchitis
Furthermore, bronchitis can have various forms of progression, including acute and chronic. Some people may have a heightened tendency to recurring forms of bronchitis due to the characteristics of their bodies or environmental conditions. Studying these unusual aspects of the disease helps to better understand the mechanisms of the onset and progression of bronchitis, which in turn contributes to the improvement of diagnostic and treatment methods for this disease.