Celiac disease: symptoms, diagnosis, and treatment options
- Understanding Celiac Disease: Key Aspects and Facts
- Etiology of celiac disease: main development factors
- Celiac disease symptoms: what you need to know
- Expert opinions on celiac disease treatment
- Diagnosis of celiac disease: methods and approaches
- Celiac Disease Treatment: Approaches and Methods
- Celiac disease prevention: important aspects
- Unusual facts about celiac disease
- FAQ
Understanding Celiac Disease: Key Aspects and Facts
Celiac disease, also known as gluten intolerance, is a chronic autoimmune disorder triggered by the impact of gluten on the mucosa of the small intestine in genetically predisposed individuals. This leads to the destruction of the intestinal villi, resulting in reduced nutrient absorption and the development of various symptoms.
The main aspects of understanding celiac disease include its high prevalence, the possibility of diagnosis using antibodies and biopsy of the small intestine mucosa, as well as the effectiveness of treatment through the exclusion of gluten from the diet and subsequent restoration of the intestinal mucosa.
Etiology of celiac disease: main development factors
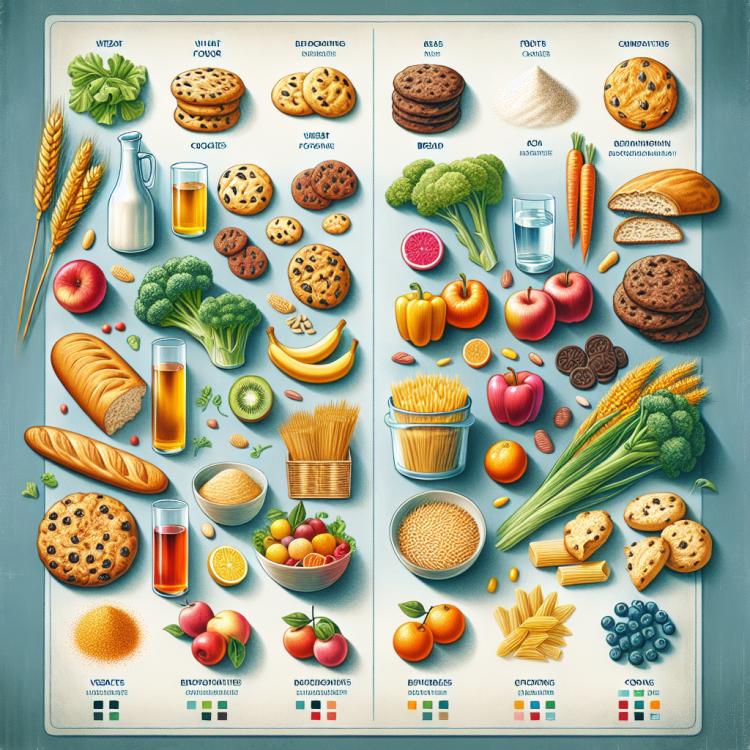
Celiac disease, a chronic immunopathological condition caused by gluten intolerance, is a protein found in wheat, rye, and barley. The primary cause of celiac disease development is an immunological reaction to gluten, leading to inflammation of the intestinal mucosa, damage to the villous epithelium, and impaired nutrient absorption.
In addition to hereditary predisposition, environmental factors, the introduction of gluten in infant nutrition, and bacterial factors may also influence the development of celiac disease. Research continues to expand our knowledge of this pathology, allowing for improved diagnosis and treatment effectiveness.
- Genetic predisposition: The presence of certain genetic mutations related to the immune system increases the likelihood of developing celiac disease.
- Immune reaction to gluten: Celiac disease occurs due to an inadequate immune response to the consumption of food containing gluten.
- Environmental factors: Environmental factors, such as bowel diseases or infections, can contribute to the development of celiac disease.
- Gluten consumption at an early age: Introducing gluten-containing foods at an early age in some individuals is associated with an increased risk of developing celiac disease.
- Intestinal dysbiosis: Disruptions in the bacterial balance in the gut can contribute to pathological processes, including celiac disease.
Celiac disease symptoms: what you need to know
The symptoms of celiac disease can vary depending on the patient’s age, the degree of damage, and individual characteristics. In adults, diarrhea, abdominal pain, bloating, weight loss, and fatigue are often observed. In children, the symptoms can be diverse, including delayed growth and mental development, anemia, irritability, skin rashes, and changes in stool.
The awareness of the medical community and the public about the various manifestations of celiac disease is of primary importance, as it facilitates timely diagnosis and the initiation of effective treatment for this pathological condition.
- Diarrhea: Frequent and excessive stool can be one of the first signs of celiac disease due to malabsorption of nutrients.
- Abdominal pain: Some patients may experience pain or discomfort in the abdominal area due to inflammation of the intestinal mucosa.
- Bloating: Observed abdominal bloating may be a result of gas formation in the intestine due to digestive disorders.
- Fatigue: Chronic fatigue and weakness may be linked to malabsorption of essential nutrients.
- Skin rashes: Some patients with celiac disease may develop skin rashes related to immune reactions to gluten.
Expert opinions on celiac disease treatment
Experts in the field of medicine dealing with celiac disease increasingly emphasize the importance of strict adherence to a gluten-free diet as the primary method of treating this condition. Individual nutrition and educating patients about proper eating habits are key aspects of successful therapy.
Moreover, modern research and medical practice focus on the potential use of pharmacological agents to treat associated symptoms of celiac disease, such as inflammation or deficiencies in certain nutrients. Discussions and defining optimal treatment strategies for celiac disease based on the latest scientific data and clinical experience are important tasks for specialists in this field.

Diagnosis of celiac disease: methods and approaches
The diagnosis of celiac disease requires a combination of clinical, laboratory, and instrumental methods. The main diagnostic method is a biopsy of the intestinal mucosa followed by histological examination, which allows for the identification of characteristic changes in the villous epithelium in celiac disease. Additionally, blood tests for antibodies to smooth muscle tissues and endomysium, stool tests for occult blood, and genetic testing for specific genetic mutations are used.
Conducting comprehensive diagnostics of celiac disease allows for an accurate diagnosis, determining the degree of intestinal damage, and prescribing appropriate treatment. Early detection and subsequent proper treatment of celiac disease help prevent complications and improve the quality of life for patients.
- Intestinal biopsy: the main diagnostic method for celiac disease, allowing the evaluation of changes in the villous epithelium.
- Blood test for antibodies: checking the levels of antibodies to smooth muscle tissues and endomysium, which may indicate celiac disease.
- Stool examination: helps to detect hidden blood, which may be a sign of intestinal damage in celiac disease.
- Genetic testing: to determine the presence of specific genetic mutations, most often associated with the development of celiac disease.
- Clinical examination and medical history: important in the diagnosis of celiac disease for identifying characteristic symptoms and risk factors in the history.
Celiac Disease Treatment: Approaches and Methods
For ordinary patients with celiac disease, if they adhere to a gluten-free diet and normalization of intestinal condition occurs, the prognosis is favorable. However, in rare cases where the diet does not provide complete relief or complications may arise, the doctor may consider the use of drug therapy, but this requires an individualized approach and monitoring by specialists.
- Gluten-free diet: exclusion of gluten-containing foods from the diet to eliminate symptoms and prevent intestinal damage.
- Nutritional support: replenishing vitamin and mineral deficiencies through special supplements if necessary.
- Medicated therapy: use of medications in rare cases when diet does not provide adequate relief, under medical supervision.
- Comprehensive medical monitoring: regular examinations and consultations with specialists for effective management of the patient’s condition.
- Individual approach: the choice of treatment methods should be based on the specific characteristics and needs of each patient with celiac disease.
Celiac disease prevention: important aspects
- Early detection of at-risk groups, such as individuals with a genetic predisposition to celiac disease or a family history of the condition.
- Monitor for signs of gluten intolerance, such as diarrhea, bloating, weight loss, fatigue, and seek medical advice when they occur.
- Awareness of celiac disease in society, which promotes early detection and initiation of treatment for the condition.
- Avoiding the consumption of gluten-containing foods in individuals at risk of developing celiac disease to prevent damage to the intestinal mucosa.
- Conducting genetic testing in relatives of patients with celiac disease for early detection and intervention if there is a genetic predisposition.
Unusual facts about celiac disease
Another interesting fact is that celiac disease is often identified in individuals of different ages, including both children and adults, which emphasizes the importance of a deep understanding of the disease among medical professionals of various specialties and the population as a whole. The detection of celiac disease among various age groups also highlights the significance of diagnosing and treating this condition for maintaining public health and improving the quality of life for patients.