Cystitis: symptoms, diagnosis, and treatment methods
Definition and causes of cystitis
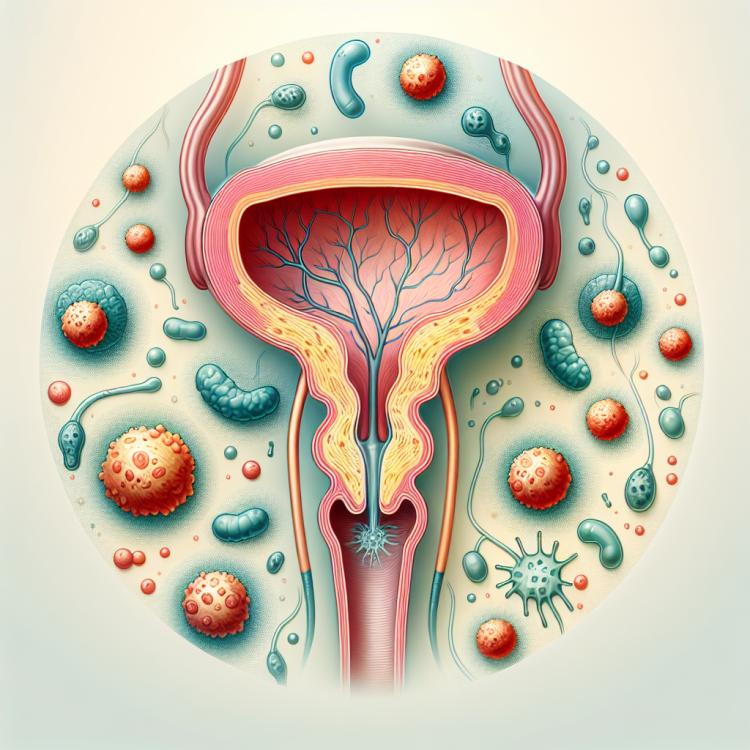
Cystitis is inflammation of the bladder, most often caused by a bacterial infection. Bacteria from the environment or the patient’s body typically enter the bladder through the urethra, leading to the development of inflammation. The main causes of cystitis include incomplete bladder emptying, urinary dysfunction, and the presence of other medical conditions that contribute to the development of infection in the bladder.
Risk factors for the development of cystitis
Cystitis, inflammation of the bladder, can be caused by various risk factors. One of the main causes is a bacterial infection, most often caused by E. coli. In women, the anatomical structure of the urinary tract facilitates easier penetration of bacteria into the bladder, which increases the likelihood of developing cystitis.
Other risk factors include a weakened immune system, the use of spermicides or pads, hormone deficiency in postmenopausal women, prolonged retention of urine, or urination during cooling, as well as individual characteristics of the body, such as allergies or anomalies in the structure of the urinary tract.
- Bacterial infection: Most often, cystitis is caused by the bacterium E.coli, which can penetrate the bladder and cause inflammation.
- Anatomical features: In women, bacteria can more easily enter the bladder due to the anatomical features of the urinary tract.
- Reduced immunity: Weakened immunity can make the body more vulnerable to infections, including cystitis.
- Use of spermicides: Chemicals in spermicides can irritate the bladder mucosa, contributing to the development of inflammation.
- Urine retention: Prolonged urine retention or incomplete emptying of the bladder can promote bacterial growth and the occurrence of cystitis.
Main signs of cystitis
Cystitis is characterized by a number of typical symptoms, including frequent urination, involuntary urination, painful urination, fever, lower abdominal pain, and changes in the nature of urine. Patients with cystitis may experience a change in urine color (for example, cloudiness) and the appearance of an unusual urine odor. Recognizing these symptoms is crucial for conducting further diagnostic and therapeutic measures.
- Frequent urination: A constant urge to urinate, even when the bladder is empty, is one of the typical signs of cystitis.
- Painful urination: A burning sensation, sharp pain, or discomfort during urination may indicate inflammation in the bladder.
- Involuntary urination: The so-called urinary incontinence can be one of the consequences of cystitis, especially with an infection of the urethra or urinary tract.
- Lower abdominal pain: Discomfort or pain in the area above the pubic bone may be associated with inflammatory processes in the bladder.
- Changes in urine: Urine in cystitis may become cloudy, have an unusual odor, or contain traces of blood, which is also an important symptom of the disease.
Expert recommendations for treating cystitis
The experts’ opinion on the treatment of cystitis is based on a comprehensive approach that includes antibiotic therapy to combat bacterial infection, abundant fluid intake to help flush the urinary tract, as well as adherence to hygiene recommendations for the genitourinary area. Effective treatment of cystitis may also include the use of anti-inflammatory medications to alleviate pain and reduce inflammation of the bladder.
Experts emphasize the importance of consulting a doctor to prescribe the optimal treatment course, considering the individual characteristics of the patient and any possible contraindications to certain medications. Preventive measures, such as maintaining a proper drinking regimen and hygiene, also play a significant role in preventing recurrences of cystitis.

Methods of diagnosing cystitis
Diagnosis of cystitis includes a variety of methods, starting with a general urine analysis, which can detect the presence of blood, protein, and bacteria in the urine. If bacterial cystitis is suspected, culture methods are used to identify the infectious agent and select the most effective antibacterial treatment. Cystoscopy, a method that uses an optical device to view the internal structure of the bladder, may be used for a more detailed study of the walls of the organ and to identify pathologies.
Additional diagnostic methods may include ultrasound examination of the bladder to assess its size and structure, as well as computed tomography to detect possible complications or other pathologies associated with cystitis. The appointment of specific diagnostic methods depends on the clinical picture of the disease and the need for a detailed study of the state of the bladder in a particular patient.
- General urine analysis: The initial stage of cystitis diagnosis, allowing for the detection of blood, bacteria, leukocytes, and other indicators characteristic of the inflammatory process in urine.
- Bacteriological urine examination: Necessary for determining the type of infection pathogen and its sensitivity to antibiotics, facilitating the choice of effective treatment.
- Cystoscopy: An instrumental diagnostic method that allows for the visual inspection of the internal surface of the bladder and the identification of changes associated with cystitis.
- Ultrasound examination: Helps to assess the size of the bladder, the presence of stones or tumors, as well as changes in the structure of the organ.
- Computed tomography: A diagnostic method used to identify complications or comorbid conditions, such as obstruction of the urinary tract or bladder diverticula.
Overview of cystitis treatment methods
In addition, anti-inflammatory medications or pain relievers may be prescribed to alleviate symptoms and speed up recovery. In cases of recurrent cystitis or complicated forms of the disease, additional examination and an individualized approach to treatment may be required. It is essential to follow the physician’s recommendations and complete the full course of treatment to avoid possible complications and prevent recurrent episodes of the disease.
- Use of antibiotics: Antibacterial medications are often used to treat cystitis to eliminate the bacterial infection.
- Abundant drinking: Drinking large volumes of liquid helps to accelerate the elimination of microorganisms from the urinary tract.
- Anti-inflammatory medications: Drugs in this group can be used to reduce inflammation and alleviate the symptoms of cystitis.
- Pain relievers: These medications can be used to relieve pain associated with cystitis.
- Additional examination and individual approach: In cases of complicated forms of cystitis or its recurrent manifestations, additional examination and the development of an individual treatment strategy may be required.
Preventive measures for cystitis
Other important measures include abundant fluid intake to stimulate the frequency of urination, avoiding hypothermia, especially in the lower back and lower abdomen, and a proper diet that includes antioxidants, which can help combat inflammatory processes. Adhering to these measures helps reduce the risk of developing cystitis and maintain the health of the urinary system.
- Maintaining hygiene of the urogenital system: Regular washing, following intimate hygiene rules, and using natural underwear help prevent the development of infections in the urinary tract.
- Timely urination: Avoiding the retention of urine helps prevent urine retention in the bladder, which can contribute to the development of infections.
- Strengthening the immune system: Proper nutrition, regular physical activity, adequate rest, and the intake of vitamins and minerals help strengthen the body and prevent the development of diseases, including cystitis.
- Avoiding hypothermia: It is especially important to protect the lower back and lower abdomen from cold, as cold contributes to a decrease in the body’s protective functions.
- Plenty of fluid intake: Drinking enough water helps reduce the concentration of bacteria in the urine and promotes frequent emptying of the bladder.
Amazing facts about cystitis
Another interesting fact is that some people may experience cystitis without obvious symptoms, which complicates diagnosis and requires special attention to risk factors. Some individuals may have a hidden form of cystitis, which can cause chronic inflammation and potential complications. Such cases emphasize the importance of regular examinations and consultations with a doctor for timely detection and effective treatment of cystitis.