Diabetic retinopathy: symptoms, diagnosis, and treatment
- Understanding Diabetic Retinopathy
- Factors contributing to the development of diabetic retinopathy
- Early signs of diabetic retinopathy
- Effective approaches to treating diabetic retinopathy
- Modern methods of diagnosing diabetic retinopathy
- Innovative methods for treating diabetic retinopathy
- Measures to prevent diabetic retinopathy
- Intriguing aspects of diabetic retinopathy
- FAQ
Understanding Diabetic Retinopathy
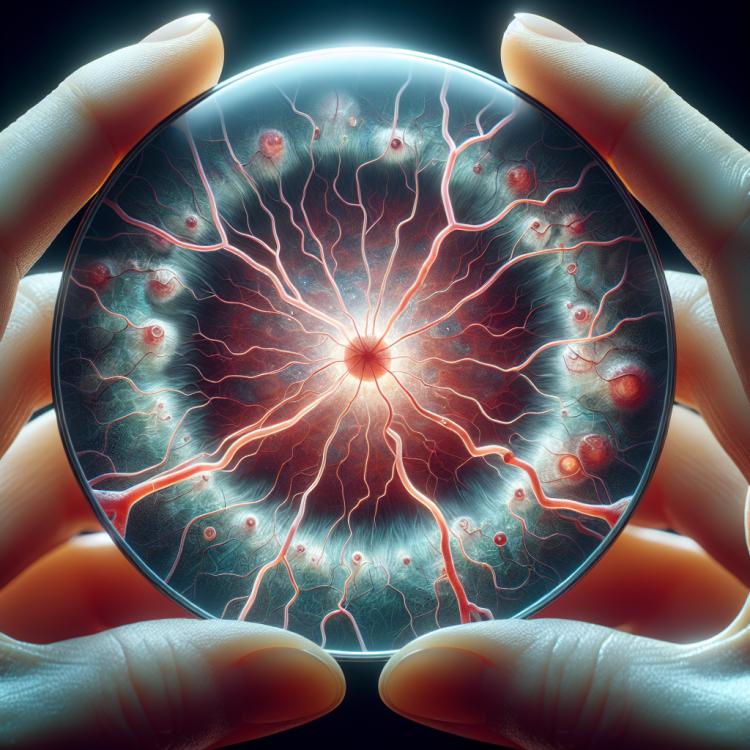
Diabetic retinopathy is a serious complication of diabetes that occurs due to damage to the blood vessels of the retina from high blood glucose levels. This process can lead to changes in blood vessels, swelling of the retina, the formation of new vessels, and hemorrhages. As a result, patients with diabetic retinopathy experience vision problems, including blurriness, poor visibility in the dark, and even loss of vision if the condition is not controlled.
Important measures in the treatment of diabetic retinopathy include maintaining stable blood glucose levels, controlling blood pressure, regular eye examinations by a specialist, and, in some cases, performing laser therapy or injections of medications into the eye. Adequate treatment and disease control help prevent the progression of diabetic retinopathy and preserve vision in patients with diabetes.
Factors contributing to the development of diabetic retinopathy
Diabetic retinopathy is a serious complication of diabetes that develops due to prolonged elevation of blood glucose levels. Hyperglycemia leads to damage to the walls of the retinal vessels, which can result in their swelling, ischemia, and neoplasms. In addition, hyperglycemia contributes to the exacerbation of inflammatory processes and the activation of growth factors that induce angiogenesis and fibrosis in the retina.
- Elevated blood glucose levels: prolonged increase in glucose levels can cause serious damage to the blood vessels of the retina.
- Arterial hypertension: increased blood pressure increases the risk of developing diabetic retinopathy.
- Vascular pathology: changes in the structure and function of the vessel walls may contribute to the development of retinopathy.
- Lipid metabolism disorders: imbalance of fats in the body can create conditions for further degeneration of blood vessels.
- Genetic predisposition: the presence of certain genetic variations may increase the risk of developing diabetic retinopathy.
Early signs of diabetic retinopathy
Early signs of diabetic retinopathy may include changes in the retinal vessels, microaneurysms, hemorrhages, and macular edema. Patients may also experience blurred vision, occasional spots in front of their eyes, and reduced vision sharpness in the dark or in low light conditions. Early signs usually do not cause pain or discomfort, so regular eye examinations are important for detecting changes at an early stage and preventing disease progression.
- Changes in retinal vessels: include dilation, constriction, and tortuosity of the vessels, which can affect blood flow and oxygen supply to the tissues.
- Microaneurysms: small bulges on the walls of capillaries, often indicating early changes in the fundus of the eye.
- Hemorrhages: bleeding may occur due to damage to capillaries and lead to changes in visual function.
- Macular edema: accumulation of fluid in the central area of the retina, which can lead to impaired vision clarity.
- Blurred vision and spots in front of the eyes: patients may experience changes in their perception of the surrounding world, which may be a sign of diabetic retinopathy.
Effective approaches to treating diabetic retinopathy
Experts in the medical field believe that effective approaches to the treatment of diabetic retinopathy include methods such as laser photocoagulation, intravitreal injections of drugs, and surgical interventions when necessary. Laser photocoagulation is used to destroy neovascularization and prevent vision deterioration; however, this method may not completely stop the progression of the disease. Intravitreal injections of anti-vascular growth factors may help with macular edema and vascular neoplasms, while surgical methods, such as vitrectomy, are used to remove blood and scar tissue from the vitreous body in advanced stages of the disease.

Modern methods of diagnosing diabetic retinopathy
Modern methods of diagnosing diabetic retinopathy include examination of the fundus using optical coherence tomography (OCT) and fluorescein angiography to assess the condition of the blood vessels and tissues of the retina. The method of ultrasound biomicroscopy is also widely used for detailed study of the structure of the anterior segment of the eye and the posterior part of the eyeball.
For more accurate determination of the degree of diabetic retinopathy, methods for assessing retinal thickness, analyzing the central macula, and studying the characteristics of vitreous opacities may be used. Many modern diagnostic methods allow for the detection of changes at early stages of the disease, which contributes to more effective control and treatment of diabetic retinopathy.
- Optical coherence tomography (OCT): allows for high-quality images of the retinal structure, detects edema and microaneurysms.
- Fluorescein angiography: provides information about the state of blood vessels, abnormalities in blood flow, and neoplasms.
- Ultrasound biomicroscopy: is used for detailed examination of the anterior and posterior segments of the eye, identifying changes in the structure and volume of the vitreous body.
- Measurement of retinal thickness: this method helps assess the thickness of the retina, which is important for evaluating the severity of diabetic retinopathy.
- Examination of the central macula: allows for detecting changes in the area of greatest visual acuity and determining the degree of macular involvement.
Innovative methods for treating diabetic retinopathy
Laser therapy is used for photocoagulating the blood vessels of the retina and slowing the progression of diabetic retinopathy. Surgical methods, including vitrectomy, may be applied in cases of serious complications such as retinal detachment. Combined treatment methods, including injections, laser therapy, and surgical interventions, often show good results in managing diabetic retinopathy.
- Anti-VEGF injections: The use of modern anti-VEGF drugs, such as Ranibizumab and Aflibercept, helps reduce bleeding and improve the condition of the retinal vasculature by inhibiting vascular endothelial growth factor.
- Laser therapy (photocoagulation): Laser treatment of the retinal blood vessels slows the progression of diabetic retinopathy and prevents further complications.
- Surgical intervention (vitrectomy): In cases of severe complications, such as retinal detachment, a vitrectomy may be required to restore visual functions.
- Combined treatment: Combined methods are often used, including anti-VEGF injections, laser therapy, and surgical interventions for effective management of diabetic retinopathy.
- Telemedicine technologies: Modern medicine actively utilizes telemedicine technologies for remote monitoring of the eye condition in patients with diabetic retinopathy and timely treatment initiation.
Measures to prevent diabetic retinopathy
Important aspects of preventing diabetic retinopathy also include a healthy diet, physical activity, avoidance of harmful habits (smoking, alcohol consumption), and regular medical check-ups for the early detection and monitoring of eye health. The timely initiation of preventive measures and adherence to the physician’s recommendations play a key role in reducing the risk of developing diabetic retinopathy in patients with diabetes.
- Stabilization of blood glucose levels: Regular monitoring of glycemia and adherence to dietary and medication recommendations help reduce the risk of developing diabetic retinopathy.
- Blood pressure control: Maintaining normal blood pressure reduces the risk of damage to the retinal vessels and the development of retinopathy.
- Blood lipid levels: Cholesterol and triglyceride levels should be monitored, as high lipid levels may contribute to the development of vascular changes in the retina.
- Healthy diet: A diet rich in fruits, vegetables, grains, fish, and lean meats helps maintain eye health and reduce the risk of developing diabetic retinopathy.
- Physical activity: Regular moderate physical activity can improve circulation and overall health, which has a positive effect on the condition of the retina.
Intriguing aspects of diabetic retinopathy
Another interesting fact about diabetic retinopathy is that treating this complication may require an integrated approach, including medication therapy, laser correction, and surgical intervention depending on the stage and severity of the damage. Regular monitoring by an optometrist or ophthalmologist, close collaboration with an endocrinologist, and adherence to healthcare recommendations play a crucial role in the successful management of diabetic retinopathy.