Diaphragmatic hernia: diagnosis, complications, and treatment methods
- Definition and causes of diaphragmatic hernia
- Etiology of diaphragmatic hernia
- Clinical picture of a diaphragmatic hernia
- Expert opinion on methods for treating diaphragmatic hernia
- Methods for diagnosing diaphragmatic hernia
- Methods of treating diaphragmatic hernia
- Methods of preventing diaphragmatic hernia
- Interesting aspects of diaphragmatic hernia
- FAQ
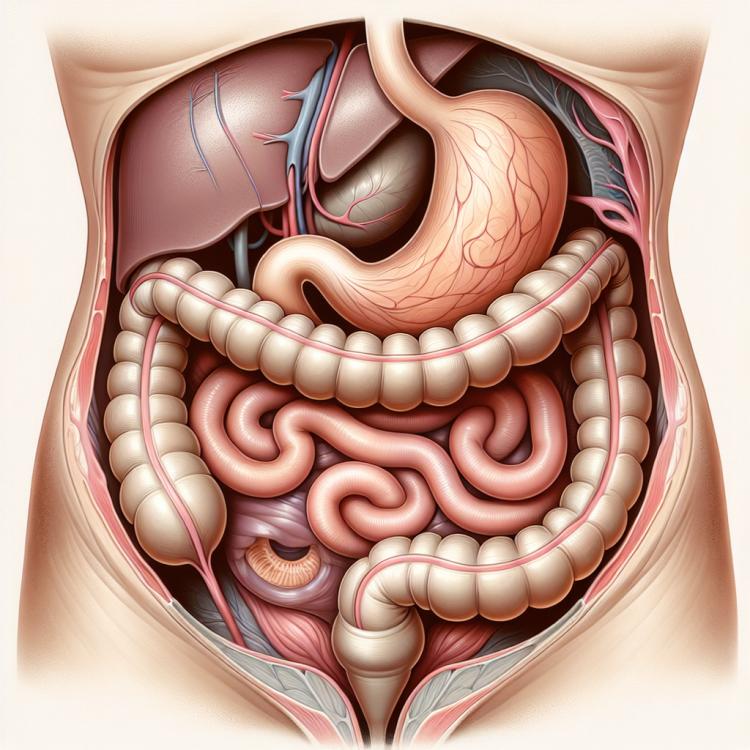
Definition and causes of diaphragmatic hernia
A hiatal hernia is a condition where organs protrude from the abdominal cavity through an opening in the diaphragm that is normally intended for the passage of the esophagus. This can occur due to weakness in the diaphragm muscles or the opening, allowing organs to move into the chest cavity. The causes of a hiatal hernia can be congenital or acquired, including injuries, excessive pressure in the abdominal cavity, obesity, or aging, which contribute to the weakening of diaphragm tissues.
Etiology of diaphragmatic hernia
A diaphragmatic hernia is a condition in which a weakened diaphragmatic (intercostal) muscle allows organs from the abdominal cavity to move into the thoracic cavity. The causes of this phenomenon can vary, including congenital developmental anomalies, increased pressure in the abdominal cavity due to obesity or pregnancy, trauma, or rare medical conditions such as esophagitis or connective tissue diseases. As a result of the pressure of the organs on the diaphragm, it weakens, which contributes to the development of a hernia.
- Congenital anomalies of development: Genetic factors can lead to diaphragm weakening from birth.
- Increased pressure in the abdominal cavity: Obesity or pregnancy can increase intra-abdominal pressure, contributing to the development of a diaphragmatic hernia.
- Injuries: Damage to the diaphragm due to trauma, such as a road accident, can cause its weakening and potential hernia formation.
- Esophagitis: Inflammation of the esophagus can contribute to diaphragm weakening and an increased risk of hernia development.
- Connective tissue diseases: Certain conditions, such as Marfan syndrome or Ehlers-Danlos syndrome, can lead to tissue weakening, including the diaphragm, increasing the likelihood of a diaphragmatic hernia.
Clinical picture of a diaphragmatic hernia
Hiatal hernia can manifest various symptoms, including a feeling of heaviness and pressure in the chest or abdominal area, frequent and painful heartburn, especially after eating, difficulty breathing, frequent sneezing or coughing, as well as pain in the abdominal or chest area. More serious symptoms may include vomiting, belching, difficulty swallowing, coughing up blood, or involuntary weight loss. It is important to see a doctor if a hiatal hernia is suspected, as these symptoms may also indicate other serious conditions and require professional evaluation.
- Feeling of heaviness and pressure: patients may experience discomfort and pressure in the chest or abdominal area.
- Heartburn: frequent and intense burning sensation in the chest area, especially after eating, may be a symptom of a diaphragmatic hernia.
- Respiratory disorders: difficulty breathing may be observed in patients with a diaphragmatic hernia due to organ pressure on the lungs.
- Sneezing or coughing: frequent sneezing or coughing may also be related to a diaphragmatic hernia, caused by irritation of the diaphragm.
- Pain and discomfort: patients may complain of pain in the abdominal or chest area, especially after eating or during physical activity.
Expert opinion on methods for treating diaphragmatic hernia
Expert opinions on the methods of treating diaphragmatic hernia emphasize the importance of an individual approach to each patient, considering the severity of symptoms, the presence of complications, and overall health status. Experts note that in some cases, conservative methods, such as lifestyle changes, regular exercises to strengthen muscles, and following a special diet, can be quite effective, especially for small hernias.
However, in cases where the diaphragmatic hernia leads to severe symptoms or complications, experts recommend surgical intervention. Modern surgical techniques, such as laparoscopic hernia repair, allow for effective correction of the diaphragmatic hernia, reducing the risk of complications and ensuring quick recovery for the patient after surgery.

Methods for diagnosing diaphragmatic hernia
The diagnosis of a diaphragmatic hernia includes various methods, including X-ray of the stomach with barium food, computed tomography (CT), or magnetic resonance imaging (MRI) to visualize the hernia and assess its size and location. Endoscopy may be used to evaluate the condition of the esophagus and stomach, especially in the presence of symptoms of reflux of stomach contents. Additional methods, such as esophageal manometry and fluoroscopy, may be applied for further assessment of the functional state of the digestive system and diaphragm.
- Barium swallow X-ray: a procedure that allows visualization of the passage of food from the esophagus to the stomach, identifying the presence of a hiatal hernia.
- Computed tomography (CT): a method using X-rays to create detailed images of internal organs, helping to identify the presence of a hernia and assess its characteristics.
- Magnetic resonance imaging (MRI): a more detailed method of visualizing internal organs using magnetic fields, which can be applied for diagnosing a hiatal hernia.
- Endoscopy: a procedure that allows a visual assessment of the condition of the esophagus and stomach, which can be useful when suspicion of a hiatal hernia arises.
- Esophageal manometry: a method of measuring pressure in the esophagus, which can be useful for assessing functional status when suspecting a hiatal hernia.
Methods of treating diaphragmatic hernia
- Diet and lifestyle changes: Includes avoiding excessively spicy, fatty, or acidic foods, moderate portion sizes during meals, and raising the head of the bed while sleeping.
- Medication therapy: The use of medications to reduce negative symptoms such as heartburn and possible reduction of stomach acidity.
- Surgical intervention: Surgical treatment may be required in cases where conservative methods do not provide adequate relief or in the presence of complications.
- Therapeutic exercise: Special exercises and physical therapy can help strengthen the abdominal muscles and improve diaphragm support.
- Psychological support: In cases of prolonged and severe disease progression, the assistance of a psychologist or support from loved ones can contribute to the psycho-emotional well-being of the patient.
Methods of preventing diaphragmatic hernia
- Maintaining a healthy weight: Excess weight can increase pressure in the abdominal cavity, contributing to the development of a diaphragmatic hernia.
- Moderate physical exercise: Regular exercises, such as yoga or Pilates, can help strengthen the muscles of the abdominal wall and diaphragm, reducing the risk of hernia.
- Proper nutrition: Consuming healthy and balanced food rich in fiber and natural products promotes digestive system health and can help prevent the development of a hernia.
- Avoiding overeating: Regular small portions of food can help prevent increased pressure in the abdominal cavity.
- Refraining from smoking: Smoking can worsen symptoms and complicate the treatment of a diaphragmatic hernia, so it is important to avoid this habit for disease prevention.
Interesting aspects of diaphragmatic hernia
An interesting fact is that lifestyle and diet can also play a key role in the onset and severity of diaphragmatic hernia symptoms. Factors such as excess weight, insufficient physical activity, excessive use of nicotine and alcohol, as well as improper nutrition, can increase the likelihood of developing or worsening hernia symptoms. Thus, effective prevention and treatment may include not only medical methods but also lifestyle and dietary adjustments.