Duodenitis: diagnosis, treatment, and recommendations
Understanding duodenitis: key aspects, symptoms, and diagnosis
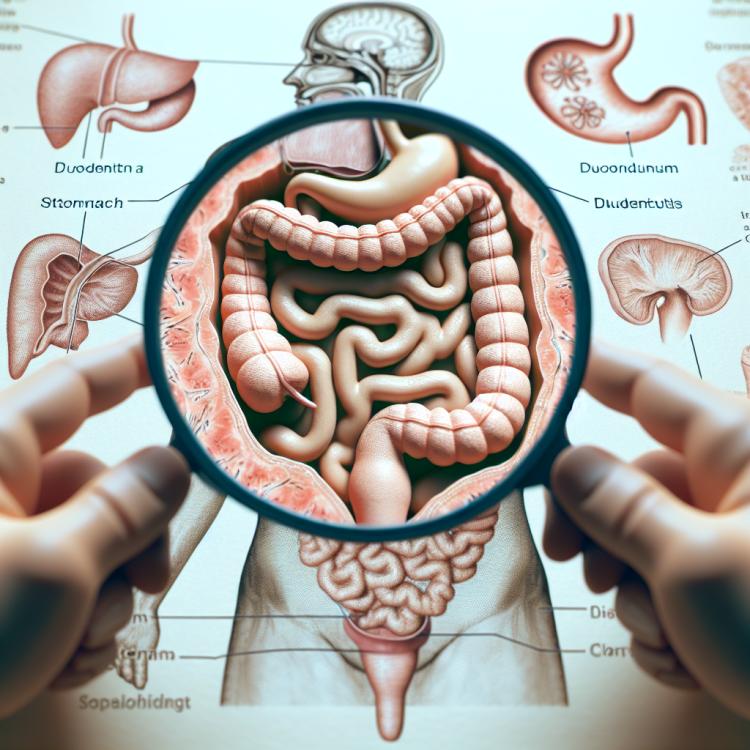
Duodenitis is an inflammatory disease of the duodenal lining, often caused by a Helicobacter infection or exposure to uncontrolled factors such as stress and the use of certain medications. The main symptoms of duodenitis include pain or discomfort in the epigastric area, heartburn, belching, nausea, and rarely vomiting. To diagnose the disease, an endoscopic examination with a biopsy of the mucosa is necessary, which will help determine the degree of inflammation and rule out possible complications.
Etiology of duodenitis
Duodenitis, as an inflammatory disease of the duodenal region of the gastrointestinal tract, can have various causes, including infections, gastroesophageal reflux, stress, alcohol consumption, and certain medications. Nutritional disorders, irritants in food, allergies, and other factors can also contribute to the development of duodenitis. It is important to conduct a thorough examination of patients to determine the specific etiology of the disease and prescribe appropriate treatment, taking into account the individual characteristics of each case.
- Infections: bacteria, viruses, or fungi, such as Helicobacter pylori, can cause inflammation of the duodenum.
- Gastroesophageal reflux: regurgitation of stomach contents into the esophagus can irritate the mucous membrane of the duodenum.
- Stress and digestive disorders: increased stress levels or digestive disorders can contribute to the development of duodenitis.
- Alcohol and certain medications: consumption of alcohol or certain medications can irritate the mucous membrane of the duodenum.
- Food allergens and irritants: some foods, chemical additives, or allergens can contribute to inflammation in the duodenal area.
Clinical picture of duodenitis
The clinical picture of duodenitis often includes symptoms such as pain or discomfort in the epigastrium, nausea, vomiting, heartburn, belching, as well as stool disturbances. Patients may experience discomfort after eating, especially spicy, fried, or fatty foods. Symptoms of duodenitis may often arise or worsen at night or on an empty stomach, but can also manifest at other times of the day.
This pathology can lead to general weakness, a decrease in appetite, and weight loss in the patient. An accurate diagnosis requires the conduction of medical research and examinations, as well as consultations with specialists to identify specific symptoms and develop further treatment strategies.
- Epigastric pain: pain or discomfort in the epigastric area (upper part of the abdomen) is often one of the first and most common symptoms of duodenitis.
- Nausea and vomiting: patients with duodenitis may experience feelings of nausea and episodic vomiting, especially after eating.
- Heartburn: a burning sensation or heartburn in the chest area may also be one of the accompanying symptoms of this disease.
- Belching: frequent or excessive belching may be observed in patients with duodenitis, especially after eating.
- Bowel disturbances: changes in bowel movements, such as diarrhea or constipation, may occur in connection with duodenitis due to changes in the digestive system’s function.
Expert opinion on the treatment of duodenitis
When treating duodenitis, it is important to consider the individual characteristics of each patient, as well as the main principles of treating this disease. Experts recommend using a comprehensive approach that includes the use of medications to improve digestion, reduce the acidity of gastric juice, and combat possible infection. At the same time, it is important to adjust the diet and lifestyle, excluding spicy, fried, and fatty foods, as well as refraining from smoking and consuming alcohol.
Experts also emphasize the significance of regular monitoring and long-term observation of patients with duodenitis to prevent exacerbations and the development of complications. They recommend following the doctor’s recommendations, prescribing a course of therapy, and regular consultations with specialists for effective management of this condition and maintaining the patient’s stable state.

Methods of diagnosing duodenitis
The diagnosis of duodenitis includes various research methods to determine the presence and nature of the inflammatory process in the duodenum. The key diagnostic methods include endoscopy of the upper gastrointestinal tract with the collection of biopsy material for histological analysis, gastroscopy, X-ray of the abdominal organs, and duodenal intubation. In addition, laboratory tests, such as blood, stool, and urine analyses, can aid in establishing the diagnosis and assessing the degree of inflammation.
Additional diagnostic methods, such as computed tomography and ultrasound examination of the abdominal cavity, may be used to identify possible complications of duodenitis and evaluate the condition of the surrounding tissues. After accurate diagnosis of signs of duodenitis, it is important to begin prescribing appropriate treatment, taking into account the specifics of the particular case of the disease and the source of inflammation.
- Esophagogastroduodenoscopy: an endoscopic method that allows for the visual examination of the mucous membrane of the digestive tract.
- Biopsy: taking a tissue sample for subsequent histological analysis to identify inflammation and other pathologies.
- Gastroscopy: a method of examining the upper parts of the digestive system using a special flexible instrument.
- X-ray of the abdominal organs: radiological examination to identify changes and pathologies in the stomach and intestines.
- Duodenal intubation: a procedure that allows for the collection of gastric juice and intestinal contents for analysis.
Treatment of duodenitis
It is important to individualize treatment considering the peculiarities of each patient, the severity of the disease, and the presence of complications. Regular monitoring by a physician, adjustments to recommendations, and support from specialists will help achieve effective control over duodenitis and improve the patient’s quality of life.
- Diet: An important part of the treatment of duodenitis is following a diet that excludes irritating foods such as fatty, spicy, and acidic dishes.
- Anti-inflammatory medications: The prescription of medications that help reduce inflammation and alleviate the symptoms of the disease.
- Antibacterial therapy: If necessary, treatment is conducted with medications to eliminate possible infection and prevent its spread.
- Acid-reducing medications: The use of medications that reduce the acidity of gastric juice to protect the mucous membrane of the duodenum.
- Supportive therapy: In some cases, additional treatment may be required to eliminate symptoms, such as anti-Helicobacter therapy or medications to inhibit acid production.
Prevention of duodenitis
Very important elements of duodenitis prevention include maintaining a work and rest schedule, combating stress, leading an active lifestyle, giving up bad habits, timely initiation of treatment for gastroesophageal reflux, and recovery after taking antibiotics and other medications. Regular medical check-ups, monitoring the condition of the gastrointestinal tract, and consulting a doctor at the first signs of digestive disorders will help to timely identify and prevent the development of the disease.
- Proper nutrition: incorporating fresh fruits, vegetables, whole grains, and dairy products into the diet helps normalize the functioning of the gastrointestinal tract and prevents irritation of the duodenum mucosa.
- Avoiding irritants: excluding spicy, fatty, and smoked dishes, alcohol, coffee, as well as monitoring the intake of medications that cause stomach irritation, helps prevent inflammatory processes in the duodenal area.
- Regular physical activity: engaging in sports and physical exercises promotes overall health, stimulates digestion, and prevents stagnation in the gastrointestinal tract.
- Psycho-emotional balance: managing stressful situations, learning relaxation techniques, and maintaining a positive attitude contribute to the improvement of the digestive system’s functioning.
- Regular medical check-ups: timely visits to a doctor for preventive examinations and monitoring the condition of the gastrointestinal tract help detect disorders at early stages and prevent the development of diseases, including duodenitis.
Interesting facts about duodenitis
Additionally, an interesting fact about duodenitis is its impact on patients’ quality of life, primarily due to the chronicity and possible recurrent nature of the disease. This pathological condition requires prolonged and meticulous treatment, as well as continuous monitoring by physicians to prevent potential complications and reduce the risk of recurrences.