Bicornuate uterus: diagnosis, complications, and treatment methods
- Description of a bicornuate uterus: causes, symptoms, and diagnosis
- Etiology of a bicornuate uterus
- The clinical picture of a bicornuate uterus
- Expert recommendations for the treatment of bicornuate uterus
- Methods for diagnosing a bicornuate uterus
- Methods for treating a bicornuate uterus
- Preventive measures for a double-horned uterus
- Unusual about the bicornuate uterus
- FAQ
Description of a bicornuate uterus: causes, symptoms, and diagnosis
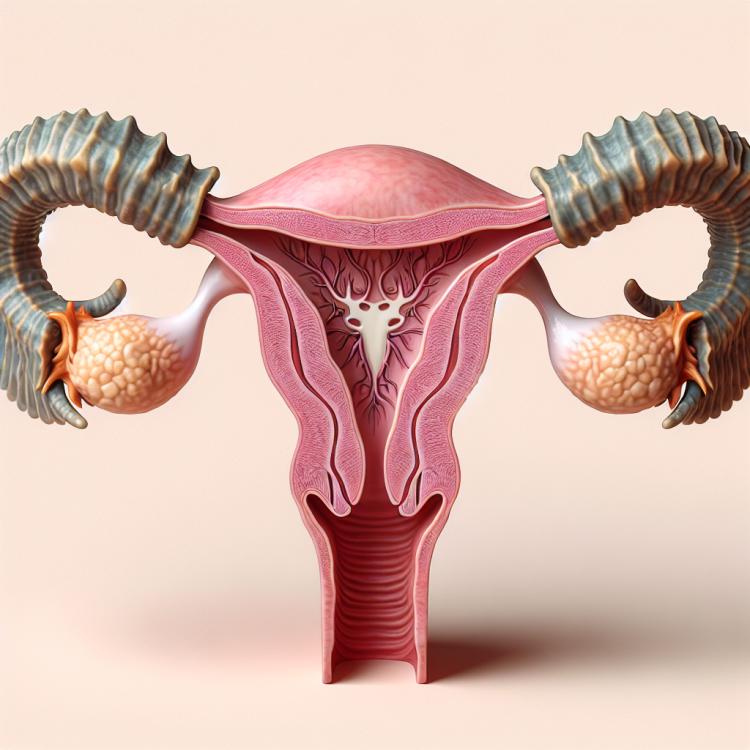
Bicornuate uterus, or uterus didelphys, is a congenital anomaly of the development of the female reproductive organ, where the uterus is divided by a vertical septum into two separate cavities. The causes of this condition can include genetic factors, disruptions during embryonic development, as well as hereditary factors.
Symptoms of a bicornuate uterus may vary, including painful menstruation, abnormal fetal positioning during pregnancy, and an increased risk of complications during childbirth. To diagnose this condition, a thorough medical history, physical examination, ultrasound, and, in some cases, magnetic resonance imaging may be required.
Etiology of a bicornuate uterus
The causes of the development of a bicornuate uterus can be diverse and vary from genetic factors to the influence of external agents on fetal development in the womb. Genetic mutations and changes in embryonic development can lead to defects in the structure of the uterus, including the bicornuate shape. External factors, such as exposure to toxic substances or radiation at various stages of pregnancy, can also affect the formation of the uterus.
Studying the causes of a bicornuate uterus is important for understanding the mechanisms of its occurrence and development. Further research in the fields of genetics, embryology, and pathology may contribute to identifying more precise causes and factors influencing the formation of a bicornuate uterus in women.
- Genetic mutations: Hereditary changes can influence the formation of the uterus, including the development of a bifid uterus.
- Exposure to toxic substances during embryonic stage: The exposure to toxins on the developing fetus can lead to defects in the structure of the uterus.
- Changes during the embryonic development process: Disruptions in the sequence of developmental processes in the fetus can lead to anomalies in the formation of the uterus.
- Immunological factors: Uncontrolled immune reactions can also affect the development of a bifid uterus.
- Exposure to radiation: Radiation exposure can negatively impact the development of the fetus, including the formation of a bifid uterus.
The clinical picture of a bicornuate uterus
The clinical picture of a bicornuate uterus can manifest with various symptoms, including painful menstruation (dysmenorrhea), pathological discharge, pain in the lower abdomen, and irregular menstrual cycles. Some women with a bicornuate uterus may experience complications during pregnancy, such as miscarriage or placenta previa. The severity of symptoms usually depends on the specific anatomical features of the bicornuate uterus, such as obstacles to the normal flow of menstrual bleeding or fetal growth in the case of pregnancy. For an accurate diagnosis and resolution of potential complications, it is essential to consult a qualified gynecologist.
- Painful menstruation (dysmenorrhea): Women with a bifid uterus often experience pain during menstruation due to the anatomical features of the uterus.
- Pathological discharge: Some women with a bifid uterus may notice unusual discharges, which may be related to changes in the structure of the uterus.
- Abdominal pain: Characteristic lower abdominal pain may accompany a bifid uterus and can occur not only during menstruation but also at other times in the cycle.
- Irregular menstrual cycle: Changes in the anatomy of the uterus can cause irregular menstrual cycles in women with a bifid uterus, with periods of high and low fertility.
- Pregnancy complications: Women with a bifid uterus may face complications during pregnancy, such as miscarriage, placenta previa, or inadequate fetal development.
Expert recommendations for the treatment of bicornuate uterus
The issue of treating a bicornuate uterus requires a comprehensive approach and an individualized plan developed with the participation of specialists in obstetrics and gynecology. Experts recommend taking into account the characteristics of each case when choosing a treatment method, considering the patient’s age, symptoms, desire for pregnancy, degree of uterine deformity, and other factors. In some cases, surgical intervention may be necessary to correct the anomaly, especially in the presence of complications.
It is important to emphasize that discussing the treatment strategy with experts and making an informed decision based on evidence-based medicine is key to effectively managing a bicornuate uterus. Experts urge patients to consult qualified specialists for all issues related to the diagnosis and treatment of this condition, in order to provide the best possible care and outcomes in their unique clinical situations.

Methods for diagnosing a bicornuate uterus
Diagnosis of a bicornuate uterus includes various methods, starting with an examination by a gynecologist and a medical history to identify possible symptoms and complaints. To confirm the diagnosis, a pelvic ultrasound may be performed, which can reveal structural anomalies of the uterus. Sometimes, for a more accurate determination of the shape of the uterus and assessment of possible defects, magnetic resonance imaging (MRI) or hysterosalpingography (hysteroscopy with contrast of the uterine cavity and tubes) may be conducted.
Diagnosing a bicornuate uterus is important for the correct choice of treatment method and for predicting the outcome. Knowing the exact diagnosis allows the doctor to develop an individual treatment plan, taking into account the specifics of each particular situation, which helps in effectively addressing potential complications and preserving the patient’s health.
- Examination and history taking: A gynecologist conducts an examination and gathers medical history to identify symptoms and complaints, as well as any preceding conditions or diseases.
- Ultrasound examination of the pelvic organs: Allows visualizing the structure of the uterus and detecting anomalies, including a bicornuate shape, as well as assessing the condition of other organs in the pelvic area.
- Magnetic resonance imaging (MRI): Clarifies the shape of the uterus, identifies possible defects, and assists in the accurate diagnosis of a bicornuate uterus.
- Hysterosalpingography: An examination in which a contrast agent is introduced into the uterine cavity and tubes, allowing the evaluation of anomalies and pathologies.
- Hysteroscopy: A diagnostic method in which a flexible tube with a video camera is inserted into the uterus, allowing for direct examination of the uterine cavity and identification of anomalies.
Methods for treating a bicornuate uterus
An individualized approach to the treatment of a bicornuate uterus may include consultation with a gynecologist-reproductive specialist or a gynecologic surgeon to make decisions about the most appropriate treatment methods. When choosing a treatment method, not only the structure and anomalies of the uterus are taken into account, but also the desires and plans of the patient regarding pregnancy and the preservation of reproductive health.
- Conservative treatment: Includes the use of hormonal medications to regulate the cycle and reduce pain during menstruation.
- Surgical intervention: In cases of serious complications and the need to correct uterine anomalies, surgery may be required.
- Medication therapy: Sometimes, medications are used to improve symptoms and reduce dysfunctional uterine bleeding.
- Hormonal therapy: The use of hormones can help stabilize uterine function and reduce the risk of complications.
- Consultation with specialists: The patient may need to consult with a reproductive gynecologist or a gynecological surgeon to choose the optimal treatment method.
Preventive measures for a double-horned uterus
A healthy lifestyle, physical activity, and proper nutrition can contribute to a woman’s overall health and reduce the risk of complications and symptoms associated with a bicornuate uterus. In the presence of genetic factors influencing the occurrence of this anomaly, consultation with a geneticist and discussion of family history may help determine an individual prevention and monitoring plan for uterine health.
- Regular check-ups: Women at risk of developing a bicornuate uterus are advised to have regular check-ups with a gynecologist for timely detection of anomalies in the structure of the uterus.
- Healthy lifestyle: Maintaining a healthy lifestyle, including proper nutrition, physical activity, and avoiding harmful habits, can promote overall health for women and reduce the risk of complications associated with a bicornuate uterus.
- Pregnancy planning: Women diagnosed with a bicornuate uterus are recommended to consult a doctor before planning a pregnancy to take into account the uterine features and minimize potential complications during pregnancy.
- Genetic counseling: If there are cases of congenital uterine anomalies in the family history, consulting a geneticist can help determine potential genetic risks and develop an individual prevention plan for a bicornuate uterus.
- Education and informing: Providing information about the risks and factors influencing the development of a bicornuate uterus allows women to be aware of their health specifics and take proactive steps to maintain it.
Unusual about the bicornuate uterus
Many women, upon learning of the presence of a bicornuate uterus, experience surprise and curiosity about such a developmental anomaly of the pelvis. Studying this condition from a medical science perspective contributes not only to understanding the morphological features but also to the development of appropriate diagnostic and treatment methods, which can improve the outcomes in managing the health of women with this abnormality.