Enteritis: diagnosis, treatment, and prevention
- Definition and main characteristics of enteritis
- Etiology of enteritis development
- The clinical picture of enteritis
- Approaches to the treatment of enteritis: expert opinion
- Methods of diagnosing enteritis
- Strategies for treating enteritis
- Measures for the prevention of enteritis
- Fascinating aspects of enteritis
- FAQ
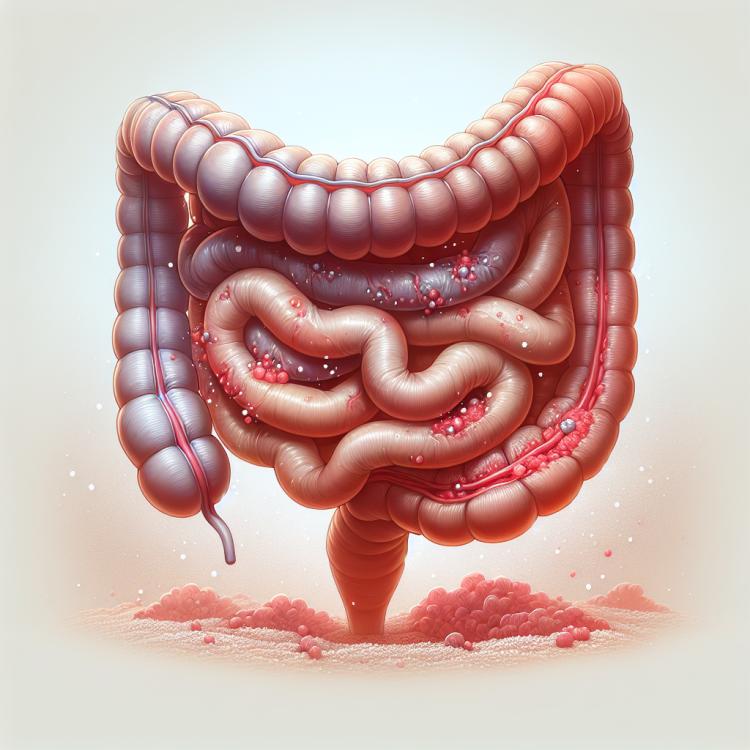
Definition and main characteristics of enteritis
Enteritis is an inflammatory disease of the small intestine, characterized by damage to its mucous membrane. The main characteristics of enteritis include symptoms such as diarrhea, abdominal pain, nausea, vomiting, general weakness, and fever. Possible causes of enteritis include infectious agents (bacteria, viruses, parasites), allergic reactions, autoimmune processes, and unbalanced nutrition. Accurate diagnosis and the selection of appropriate treatment play a key role in understanding and combating this disease, preventing possible complications.
Etiology of enteritis development
Enteritis is an inflammatory disease of the mucous membrane of the small intestine caused by various factors. The main factors contributing to the development of enteritis include viruses, bacteria, protozoa, as well as prolonged consumption of the causative agent of waterborne diseases, unfavorable hygiene conditions, and contaminated water or food. The primary pathogens are salmonella, shigella, escherichia, and other microorganisms that can penetrate the intestine through food or water, causing inflammatory processes.
In addition to infectious agents, the causes of enteritis can include autoimmune disorders, allergic reactions to certain products and medications, as well as disruptions in the immune system. In some cases, enteritis may be triggered by increased sensitivity to specific components in food. Understanding the identification of the specific cause of enteritis is crucial for effective treatment and prevention of this disease.
- Infections: Enteritis can be caused by viruses, bacteria, or protozoa, such as salmonella, shigella, and escherichia.
- Low food quality: Consumption of contaminated or tainted food can contribute to the development of enteritis.
- Autoimmune disorders: An inadequate immune system response to the body’s own tissues can lead to inflammation of the intestines.
- Allergic reactions: Some foods or medications can trigger an allergic reaction that leads to enteritis.
- Immune system dysfunction: A weakened or overactive immune system may play a role in the development of enteritis.
The clinical picture of enteritis
Enteritis manifests with a variety of symptoms related to inflammation of the intestinal mucosa. Patients may experience frequent watery stools with purulent-bloody admixtures, abdominal pain and cramps, loss of appetite, nausea, vomiting, and general weakness. Additionally, symptoms may include fever, burning and painful sensations in the abdomen, bloating, and possible signs of dehydration.
As the disease progresses, diarrhea may develop, which can be abundant and lead to rapid loss of water and electrolytes. Patients may also exhibit a possible decrease in appetite, weight loss, and in cases of severe progression – even dehydration and collapse. It is important to conduct a comprehensive examination to establish a diagnosis and timely treatment of this pathological condition.
- Frequent loose stools: patients with enteritis often experience loose stools that may contain purulent-bloody impurities.
- Abdominal pain and cramps: characteristic symptoms include abdominal pain that may have a colicky nature and spasmodic tension.
- Lack of appetite: patients often experience a decrease in appetite, which can lead to a deficiency of nutrients in the body.
- General weakness: patients may feel general weakness, fatigue, and reduced performance as a result of the inflammatory process.
- Bloating and gas formation: symptoms of abdominal bloating, increased gas formation, and discomfort in the abdomen are observed in patients with enteritis.
Approaches to the treatment of enteritis: expert opinion
Treatment of enteritis involves a comprehensive approach aimed at eliminating inflammation of the intestinal mucosa, restoring fluid and electrolyte balance, as well as alleviating the clinical manifestations of the disease. Experts recommend medical supervision over the patient’s condition, the prescription of a nutrient-rich dietary regimen, anti-inflammatory medications, and probiotics to restore the intestinal microbiota.
Particular attention should be paid to the regulation of dehydration and the elimination of diarrhea, which contribute to the recovery of the patient’s overall condition. Expert medical opinion emphasizes the importance of timely initiation of treatment, an individualized approach to each case, and subsequent monitoring of the patient to prevent complications and shorten the rehabilitation period.

Methods of diagnosing enteritis
In diagnosing enteritis, the doctor pays attention to the clinical picture of the disease, conducts a physical examination of the patient, and performs laboratory and instrumental studies. Clinical signs, such as frequent liquid stools with traces of blood or pus, abdominal pain, nausea, and general weakness, play a key role in diagnosing this condition. Laboratory tests, such as stool analysis for blood and bacteriological studies, help identify possible causative agents of infection or inflammation.
Instrumental methods include gastroscopy and colonoscopy, which allow visualization of the condition of the intestinal mucosa, identification of inflammatory changes, tumors, or other pathological processes. The diagnosis of enteritis requires a comprehensive approach, combining various examination methods to accurately determine the causes and nature of the disease, which enables the prescription of effective treatment in each specific case.
- Clinical examination: The doctor pays attention to symptoms such as watery stools with traces of blood, nausea, abdominal pain, and general weakness, which is an important step in the diagnosis of enteritis.
- Laboratory stool tests: A stool test for blood can detect the presence of hidden blood, indicating inflammatory processes in the gastrointestinal tract.
- Bacteriological studies: Allow for the identification of infection agents, such as bacteria or protozoa, which can cause the development of enteritis.
- Gastroscopy: An endoscopic method that allows for a visual assessment of the condition of the gastric and duodenal mucosa, identifying inflammatory changes or ulcerative damage.
- Colonoscopy: An examination that allows for the assessment of the condition of the colonic mucosa, detecting inflammation, ulcers, or other pathological changes associated with enteritis.
Strategies for treating enteritis
In cases of infectious etiology, antiviral or antibacterial drugs may be prescribed according to the sensitivity of the pathogen to antibiotics. Symptomatic treatment focuses on alleviating pain, controlling diarrhea, and normalizing bowel function. It is important to individualize treatment for patients, taking into account clinical features and factors that influenced the development of enteritis.
- Fluid and electrolyte compensation: elimination of dehydration through regular intake of fluids and electrolytes.
- Use of probiotics: prescription of medications to restore normal intestinal microflora after a course of antibiotics.
- Antibacterial therapy: antibacterial medications are used in case of an infectious nature of the disease.
- Symptomatic treatment: alleviation of pain syndrome and control of diarrhea for the patient’s comfort.
- Individualized approach: conducting treatment taking into account the patient’s characteristics and the causes of enteritis development.
Measures for the prevention of enteritis
Regular consumption of clean drinking water and avoiding the intake of low-quality products also play a key role in preventing enteritis. Preventive vaccinations against infections that cause this pathology can be an effective measure to reduce the risk of the disease. Effective prevention is based on a systematic approach to adhering to hygiene standards and targeted measures to control the quality of food products and water.
- Compliance with hygiene rules: regular hand washing before meals and after visiting public places reduces the risk of transmitting infections that can cause enteritis.
- Quality control of food and water: consuming clean drinking water and cooked, fried food helps prevent infections transmitted through food.
- Avoiding low-quality products: following food storage and cooking rules, as well as abstaining from raw or undercooked products, reduces the likelihood of infection with enteritis pathogens.
- Preventive vaccinations: vaccination against infections that cause enteritis can be an effective method of disease prevention.
- Public education: conducting information campaigns about measures to prevent enteritis raises awareness and promotes adherence to hygiene standards in everyday life.
Fascinating aspects of enteritis
Research on enteritis also demonstrates the impact of hygiene problems and food quality on gut health. This pathological condition can be common in countries with low sanitation and hygiene standards, which should be taken into account when developing preventive measures. It is also interesting to study the impact and effectiveness of various treatment methods for enteritis, which helps improve therapy outcomes and enhance the quality of life for patients with this condition.