Enterocolitis: symptoms, causes, and treatment methods
- Understanding Enterocolitis: Symptoms, Causes, and Treatment
- Stages of enterocolitis development
- Main symptoms of enterocolitis
- The best methods for treating enterocolitis
- Main methods of diagnosing enterocolitis
- Innovative methods of treating enterocolitis
- Modern strategies for preventing enterocolitis
- Unusual aspects of enterocolitis
- FAQ
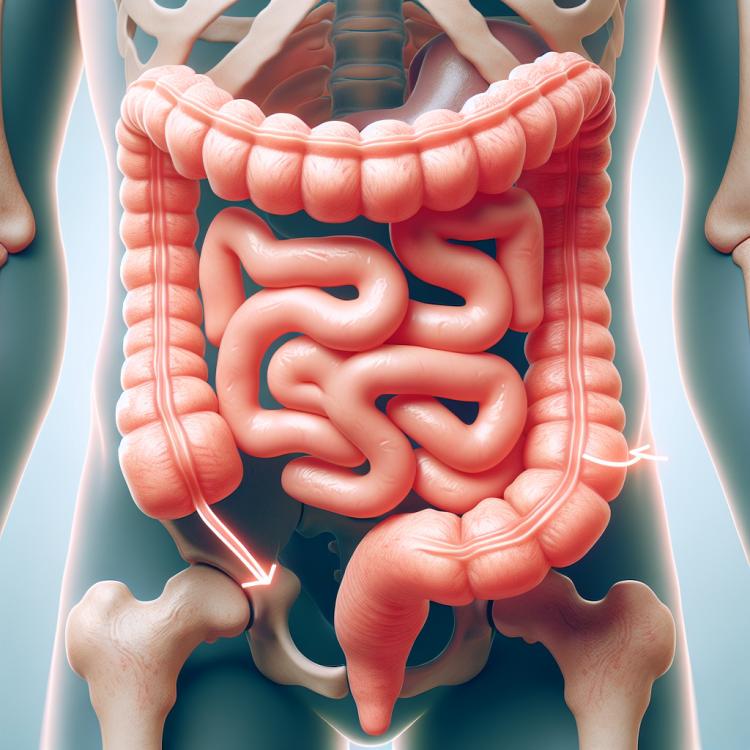
Understanding Enterocolitis: Symptoms, Causes, and Treatment
Enterocolitis is an inflammatory disease characterized by the inflammation of the mucous membrane of the small intestine and the lining of the colon. The main symptoms of this condition are abdominal pain, diarrhea with blood and mucus, as well as high body temperature. The causes of enterocolitis can be diverse, including infections, allergic reactions, autoimmune disorders, and digestive disturbances. Treatment for this disease depends on its cause and may include antibiotics, antidiarrheal medications, probiotics, diet, and other therapeutic methods.
Stages of enterocolitis development
Enterocolitis is an inflammatory disease of the intestine, most often caused by infection. Initially, there is irritation of the intestinal mucosa, leading to diarrhea and abdominal pain. In the case of prolonged illness and improper treatment, a chronic form of enterocolitis may develop, characterized by recurring episodes of intestinal inflammation, which can lead to serious complications.
- Disruption of intestinal microflora: an imbalance between “beneficial” and “harmful” bacteria can contribute to the development of inflammation.
- Inflammation of the mucous membrane: the initial stage of enterocolitis development, accompanied by diarrhea, abdominal pain, and other symptoms of intestinal inflammation.
- Development of chronic form: with inadequate treatment or insufficient control of inflammation, the condition may worsen and lead to a transition into a chronic form of the disease.
- Recurrent episodes of inflammation: characterize the chronic form of enterocolitis, requiring constant medical supervision and treatment.
- Possible complications: inadequate treatment of enterocolitis can lead to serious complications, such as bleeding, intestinal perforation, and even sepsis.
Main symptoms of enterocolitis
Enterocolitis is characterized by various symptoms, including diarrhea, blood in stool, abdominal pain, bloating, vomiting, fever, and general malaise. Diarrhea is one of the main symptoms of enterocolitis, with stools that may be excessively liquid, frequent, and may contain blood or mucus. Abdominal pain can be crampy or severe, worsening after meals and accompanied by a feeling of discomfort. The frequency, intensity, and combination of these symptoms can vary depending on the degree of inflammation and the overall condition of the patient.
- Diarrhea: one of the main symptoms of enterocolitis, manifested by excessive watery stools with traces of blood or mucus.
- Abdominal pain: can vary in nature, from cramping to intense, occurring after meals and accompanied by discomfort.
- Abdominal bloating: a feeling of fullness in the abdomen, its increase in volume, accompanied by negative sensations.
- Vomiting: the appearance of vomiting may occur as a consequence of intoxication or irritation of the gastric mucosa.
- Fever and general malaise: an increase in temperature, weakness, and fatigue may accompany enterocolitis during exacerbation.
The best methods for treating enterocolitis
Experts in the field of gastroenterology recommend a comprehensive approach to the treatment of enterocolitis, which includes the prescription of antibiotics in case of bacterial infection, the use of probiotics to restore normal intestinal microflora, as well as adherence to a special diet aimed at reducing inflammation and improving the patient’s digestion. Experts are also committed to the idea of individualizing treatment methods based on the characteristics of the source of inflammation, the stage of the disease, and the overall condition of the patient. It should be noted that successful treatment of enterocolitis requires a comprehensive approach and monitoring under the supervision of an experienced physician.

Main methods of diagnosing enterocolitis
Diagnosis of enterocolitis usually begins with a comprehensive medical history, physical examination, and analysis of symptoms such as diarrhea, abdominal pain, vomiting, and fever. Laboratory tests of blood and stool may be conducted to detect inflammatory markers, infections, or the presence of blood in the stool. Instrumental diagnostic methods, such as colonoscopy or intestinal X-rays, can help visualize changes in the intestinal mucosa, which will assist in clarifying the diagnosis and determining the extent of the damage.
- Complete blood count: can reveal signs of inflammation in the body.
- Clinical stool analysis: helps to detect the presence of blood, abnormal bacteria, or helminths in the stool.
- Bacteriological examination: allows identifying the causative agent of the infection.
- Colonoscopy: allows visualizing the condition of the intestinal mucosa and taking biopsy samples.
- Ultrasound and Radiology: can be used to assess the structure and function of the intestines.
Innovative methods of treating enterocolitis
- Use of probiotics: Probiotics help restore healthy intestinal microflora, improving digestion and the body’s protective functions.
- Immunomodulators: The use of immunomodulators strengthens immunity and helps the body fight inflammation in the intestine.
- Antibiotics: Antibiotics are prescribed to combat infections that may cause enterocolitis.
- Dietary recommendations: Specialized diets can help improve digestion and reduce inflammation in the intestine.
- Conservative methods: Physiotherapy and regular medical follow-up are important for the effective management of enterocolitis and the prevention of complications.
Modern strategies for preventing enterocolitis
- Compliance with hygiene standards: regular handwashing with soap and disinfecting surfaces with disinfectants.
- Vaccination: the use of vaccines to protect against the major pathogens of infections that cause enterocolitis.
- Intake of probiotics and preparations to normalize intestinal microflora: promotes the growth of beneficial bacteria that can prevent the development of inflammatory processes.
- Balanced diet: consuming food rich in fiber and prebiotics helps maintain intestinal health.
- Avoiding high-risk food products: one should consider the storage and preparation conditions of food, especially in countries with poor sanitary conditions.