Eye episcleritis: diagnosis, treatment, and prognosis
- Fundamentals of Episcleritis of the Eyes: Causes, Symptoms, and Diagnosis
- Factors contributing to the development of episcleritis of the eye
- Clinical manifestations of episcleritis of the eye
- Approaches to the treatment of episcleritis: a specialist’s perspective
- Methods of diagnosing episcleritis of the eye
- Therapy for Episcleritis of the eye
- Preventive measures for episcleritis of the eye
- Amazing aspects of episcleritis of the eye
- FAQ
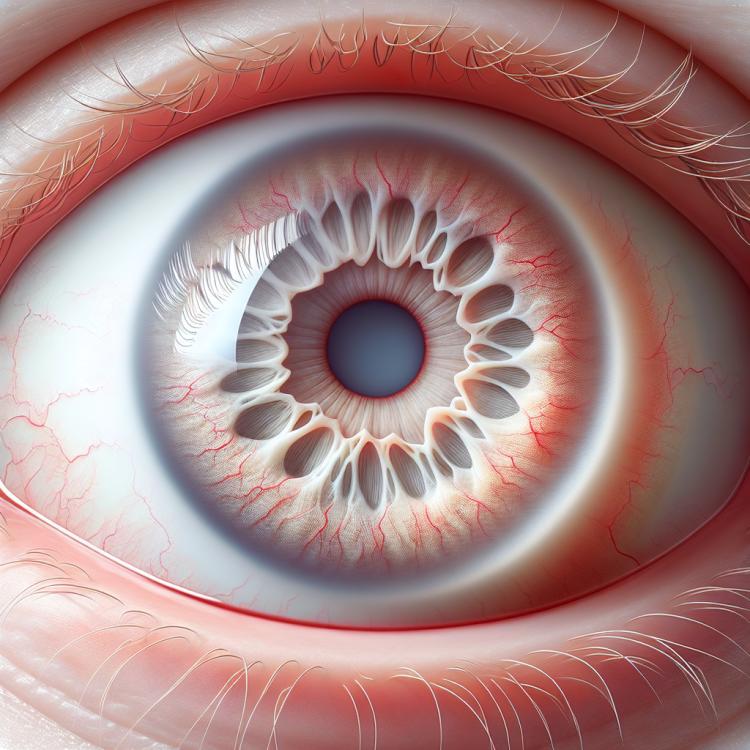
Fundamentals of Episcleritis of the Eyes: Causes, Symptoms, and Diagnosis
Episkleritis is an inflammatory disease of the eye’s sclera, symptoms of which include redness of the eyeball, a feeling of irritation, and often a painless deterioration of vision. The causes of episkleritis can be varied, including autoimmune diseases, infections, and allergic reactions. Diagnosing the disease involves an eye examination by a doctor, as well as possibly conducting laboratory tests to identify autoimmune markers or infections, which helps determine the optimal treatment plan.
Factors contributing to the development of episcleritis of the eye
Episcleritis of the eye is an inflammatory disease of the episclera, the outer layer of the eye, which is usually characterized by a localized process and lesser systemic manifestations compared to scleritis. There are several factors that may contribute to the development of episcleritis, including infections, allergic reactions, autoimmune diseases, or even stress. This type of inflammation can also be associated with other conditions, such as rheumatoid arthritis or vasculitis.
Understanding the main factors that contribute to the occurrence of episcleritis is essential for accurate diagnosis and effective treatment of this condition. Managing the causes that contribute to the development of episcleritis can reduce the risk of exacerbation and help alleviate discomfort associated with eye inflammation.
- Infections: Some viruses, bacteria, or fungi can cause inflammation of the eye’s episclera.
- Allergic reactions: Exposure to allergens can trigger an inflammatory response in the eye’s membrane.
- Autoimmune diseases: Some autoimmune conditions, such as rheumatoid arthritis or lupus, may be associated with the development of episcleritis.
- Stress: Psychological stress and emotional factors can also influence the immune system and contribute to inflammatory processes in the eye.
- Genetic factors: Heredity and genetic predispositions may play a role in the occurrence of episcleritis of the eye.
Clinical manifestations of episcleritis of the eye
Episcleritis of the eye can manifest with various clinical symptoms, including redness of the conjunctiva, which is usually not accompanied by purulent or mucous discharge. Patients may experience discomfort, a sensation of itching or burning in the eye area, as well as sensitivity to light. Vision is generally unaffected, and there are usually no pronounced systemic symptoms.
The diagnosis of episcleritis is usually based on a clinical examination, including the assessment of typical eye redness and additional methods such as biomicroscopy. A detailed examination allows for the exclusion of other potential causes of eye redness. Early detection and appropriate treatment of episcleritis can help prevent the progression of the condition into more serious forms and alleviate the patient’s symptoms.
- Redness of the eye: Episcleritis is characterized by the appearance of redness of the conjunctiva of the eye without visible purulent or mucous discharge.
- Discomfort and itching sensation: Patients often experience discomfort, a burning sensation in the eye area, and sometimes itching.
- Sensitivity to light: People with episcleritis may experience increased sensitivity to bright light (photophobia).
- Preservation of vision: Generally, the intensity of episcleritis symptoms does not affect visual functions.
- Absence of pronounced systemic symptoms: Episcleritis of the eye is usually characterized by localized manifestations and is not accompanied by general health disturbances.
Approaches to the treatment of episcleritis: a specialist’s perspective
Episcleritis of the eye requires a comprehensive approach to treatment, considering the individual characteristics of each case. Experts agree that in most cases, conservative treatment methods are used, including the application of anti-inflammatory eye drops, steroid medications, or non-drug methods such as symptom relief through cold compresses. Additionally, antihistamines or systemic medications may be prescribed in cases where necessary.
Experts emphasize the importance of an individualized approach when choosing the optimal treatment method for a specific patient. It should also be noted that in some cases, especially with comorbidities or complications, more intensive treatment or further examination may be required to achieve the best outcome and prevent recurrences.

Methods of diagnosing episcleritis of the eye
For the diagnosis of episcleritis of the eye, it is important to conduct a thorough clinical examination, including an examination by a doctor, supplemented by special instrumental methods. Biomicroscopy allows for a detailed assessment of changes in the episclera and conjunctiva, identifying characteristic signs of inflammation, and ruling out other possible causes of red eye. Additional diagnostic methods may include ultrasound scanning or magnetic resonance imaging to assess the condition of the ocular tissues.
By providing an accurate diagnosis of episcleritis of the eye, doctors can confirm the presence of an inflammatory process and determine its type and severity. This allows for consideration of the individual characteristics of each case and the prescription of effective treatment tailored to the patient’s needs, contributing to successful disease management and the prevention of potential complications.
- Clinical examination: Examination of the eye externally and internally using a biomicroscope to detect signs of inflammation on the surface of the eye.
- Biomicroscopy: An instrumental method that helps assess changes in the episclera and conjunctiva, revealing reddish discoloration of tissues characteristic of inflammation.
- Ultrasound scanning: Used for a more detailed study of the structures of the eye and to determine the condition of the ocular tissues.
- Magnetic resonance imaging: A method used to obtain high-quality images of the eye, which allows for more accurate diagnosis.
- Laboratory tests: Blood tests to detect signs of inflammation or autoimmune processes that may be associated with episcleritis of the eye.
Therapy for Episcleritis of the eye
In cases where an accompanying systemic disease, such as rheumatoid arthritis, is found, comprehensive treatment is required, taking into account the underlying disease and the inflammatory process in the eyes. Addressing factors that contribute to the development of episcleritis, such as managing allergic reactions or autoimmune processes, may also be an important component of therapy.
- Local anti-inflammatory agents: Prescribed to reduce inflammation and discomfort in the eye, such as glucocorticoid drops or ointments.
- Vasoconstrictor drops: Used to relieve redness and discomfort in the eye area.
- Comprehensive treatment for comorbid conditions: In cases of systemic diseases, an integrated approach to treatment is required, taking into account both the underlying disease and the inflammatory process in the eyes.
- Management of factors contributing to the development of episcleritis: Controlling allergic reactions, autoimmune processes, and other factors contributing to inflammation can be an important component of therapy.
- Regular monitoring of the patient’s condition: Careful monitoring of the patient’s condition and the effectiveness of treatment is necessary to prevent complications and ensure optimal treatment outcomes.
Preventive measures for episcleritis of the eye
Avoiding prolonged exposure to stress, maintaining a healthy lifestyle, including a balanced diet and physical activity, can also contribute to strengthening the immune system and reducing the likelihood of inflammatory processes in the eyes. Ventilating the room and preventing hypothermia can also help prevent the development of certain forms of inflammation of the eye membranes.
- Maintaining a work and rest schedule: Regular breaks from working on the computer or reading can help prevent eye strain and reduce the risk of inflammatory processes.
- Avoiding contact with harmful substances: When working with aggressive chemicals, it is necessary to use protective glasses or masks to avoid irritation of the eye membranes.
- Maintaining a healthy lifestyle: Regular physical exercise, healthy eating, and giving up bad habits can generally strengthen the body and immunity, which helps prevent the development of inflammatory eye diseases.
- Periodic visits to an ophthalmologist: It is recommended to undergo routine examinations by an ophthalmologist for the early detection of any changes in the condition of the eyes and timely treatment.
- Avoiding overheating or overcooling of the eyes: When working for extended periods on a computer, it is important to ensure proper lighting and avoid severe temperature fluctuations to prevent eye strain and irritation.
Amazing aspects of episcleritis of the eye
In addition to clinical aspects, discussing factors that lead to the onset of episcleritis and subsequent treatment, it is also important to consider the psychological aspect of the disease. Episcleritis can cause some anxiety in patients due to the discomfort they experience. An approach to educating about the condition, treatment, and prognosis can help patients cope with the emotional aspects of this condition.