Ethmoiditis: diagnosis, treatment, and prevention
- Understanding Ethmoiditis: Symptoms, Causes, and Treatment
- Etiology of Ethmoiditis
- Clinical picture of Ethmoiditis
- Expert opinion on the treatment of ethmoiditis
- Diagnosis methods for Ethmoiditis
- Approaches to the treatment of Ethmoiditis
- Preventive measures for Ethmoiditis
- Fascinating Aspects of Ethmoiditis
- FAQ
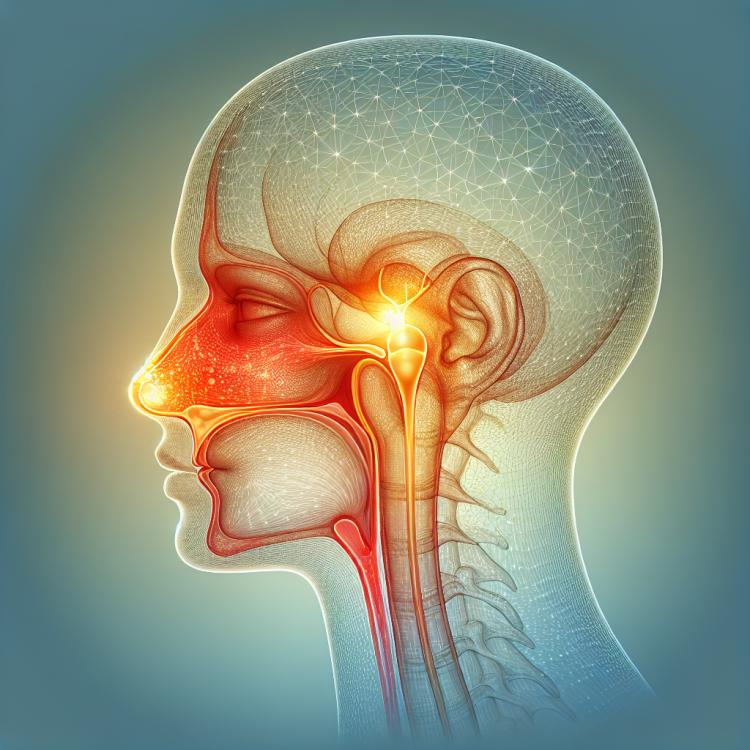
Understanding Ethmoiditis: Symptoms, Causes, and Treatment
Ethmoiditis is an inflammatory process affecting the tissue of the ethmoid sinus located in the nose. The main symptoms of ethmoiditis include nasal congestion, pain in the eye area and forehead, and disturbances in smell. The causes of ethmoiditis can include infections, allergies, and impaired drainage function of the ethmoid sinus. Antibiotics, decongestants, and sometimes surgical intervention are often used to treat ethmoiditis.
It is important to seek medical attention in a timely manner if ethmoiditis is suspected, as uncontrolled development of the inflammatory process can lead to complications. Modern treatment methods allow for effective management of ethmoiditis and the prevention of possible complications, ensuring quick recovery for the patient and preventing recurrences of the disease.
Etiology of Ethmoiditis
Ethmoiditis, an inflammatory disease of the sinuses, can have various causes. The disease is usually based on an infection caused by bacteria, viruses, or fungi. The development of ethmoiditis may also be associated with allergic reactions or anatomical features of the nasal cavity and paranasal sinuses. It is important to consider all possible risk factors and investigate their impact on the occurrence of ethmoiditis for effective treatment and prevention of this disease.
- Infections: Ethmoiditis is most often caused by a bacterial, viral, or fungal infection in the area of the ethmoid cells.
- Allergies: An allergic reaction can contribute to inflammation in the sinus area.
- Anatomical features: Deformations or narrowing of the nasal cavity and paranasal sinuses can lead to mucus stagnation and the development of ethmoiditis.
- Mucosal damage: Mechanical damage to the nasal mucosa can provoke infection and the development of ethmoiditis.
- Immunodeficiency states: A decrease in immunity increases the risk of infectious diseases, including ethmoiditis.
Clinical picture of Ethmoiditis
Ethmoiditis is often accompanied by a variety of symptoms, including breathing disorders, nasal congestion, nasal discharge, as well as pain in the forehead and eye sockets. Patients may also experience general weakness, increased body temperature, and a feeling of pressure in the forehead and nose.
Changes in psycho-emotional state, sleep and appetite disorders, as well as a decrease in smell can also be observable signs of ethmoiditis. If such symptoms appear, it is recommended to consult a doctor for diagnosis and to determine the most effective treatment.
- nasal congestion: Ethmoiditis is often accompanied by difficulty breathing due to swelling of the mucous membrane.
- Pain in the forehead and eye sockets: Patients may experience pressing or pulsating pain in the frontal and orbital areas.
- Nasal discharge: Yellowish or greenish discharge may be a symptom of sinus inflammation.
- General weakness: Ethmoiditis is often accompanied by a decline in overall well-being and fatigue.
- Fever: Some patients may experience fever due to the infectious process.
Expert opinion on the treatment of ethmoiditis
Expert opinion regarding the treatment of ethmoiditis emphasizes the importance of a comprehensive approach to therapy. Specialists recommend the individual selection of treatment methods depending on the severity of the disease, possible complications, and patient characteristics. Treatment of ethmoiditis may include the use of antibiotics, anti-inflammatory drugs, local vasoconstrictors, as well as physiotherapeutic procedures.
Experts highlight the significance of regular monitoring of the patient after the completion of treatment to prevent recurrences and to control the condition of the mucous membrane and paranasal sinuses. In addition to medication therapy, specialists may also recommend surgical intervention in complicated cases of ethmoiditis.

Diagnosis methods for Ethmoiditis
Diagnosis of ethmoiditis involves a set of activities aimed at determining the presence and nature of the inflammatory process in the area of the ethmoid cells. Clinical examination, medical history, and obstetric data are the initial diagnostic methods that allow the physician to establish a preliminary diagnosis.
Additional diagnostic methods may include computed tomography (CT) or magnetic resonance imaging (MRI) of the nasal and paranasal sinuses, radiological examination, as well as laboratory tests to identify the infectious agent. Accurate and timely diagnosis plays a crucial role in prescribing effective treatment for ethmoiditis.
- Clinical examination: The doctor conducts a visual examination of the nose and paranasal sinuses, takes the medical history, paying attention to characteristic symptoms and the patient’s complaints.
- Computed tomography (CT): Allows obtaining detailed images of the nasal area and paranasal sinuses, identifying inflammation and determining the extent of tissue damage.
- Magnetic resonance imaging (MRI): Used for a more detailed study of the structures and tissues in the nasal area and paranasal sinuses.
- X-ray examination: May be performed for additional detection of changes in the nasal area and paranasal sinuses.
- Laboratory tests: Include blood tests, swabs from the nose or throat for infection agents, which helps determine the cause of the inflammatory process.
Approaches to the treatment of Ethmoiditis
In some cases, with complicated or chronic forms of ethmoiditis, surgical intervention may be required. Surgical treatment can include bypass procedures to restore sinus drainage and removal of affected tissue. The decision regarding the need for surgery is made by the doctor after analyzing clinical data and examination results of the patient.
- Conservative treatment methods: Include the use of nasal sprays, antibiotics, and anti-inflammatory medications to reduce inflammation and symptoms.
- Physiotherapeutic procedures: May be used to improve drainage and reduce swelling of the mucous membrane.
- Vasoconstrictor drops: Are used to reduce swelling and improve nasal breathing.
- Surgical intervention: In some cases, surgery may be required to restore drainage of the paranasal sinuses and remove affected tissue.
- Individual approach: Treatment of ethmoiditis should be tailored to the individual characteristics of the patient and the nature of the disease.
Preventive measures for Ethmoiditis
To prevent ethmoiditis, it is also recommended to avoid possible allergens that affect the nasal mucosa and cause inflammation, as well as to promptly treat any infections of the upper respiratory tract to prevent their spread to adjacent areas. Regular visits to a doctor for monitoring the condition of the nasopharynx and timely detection of the initial signs of inflammation can also help in preventing the development of ethmoiditis.
- Observance of personal hygiene rules: regularly wash your nose and hands after contact with potential sources of infection.
- Conducting wet cleaning: regular cleaning of the premises will help avoid the accumulation of dust and allergens, which can contribute to inflammation of the mucous membranes.
- Avoiding unfavorable conditions: try not to get chilled or overheated, and also avoid prolonged stays in polluted or crowded rooms.
- Strengthening immunity: maintain a healthy lifestyle, including a balanced diet, sufficient physical exercise, and avoiding harmful habits.
- Timely treatment of infections: when symptoms of ARVI or other upper respiratory infections appear, consult a doctor for timely treatment and prevention of complications.
Fascinating Aspects of Ethmoiditis
In the management and timely treatment of ethmoiditis, the prevention of recurrences and complications plays an important role. Regular visits to the doctor for examinations, adherence to hygiene rules, and strengthening the immune system can reduce the risk of developing ethmoiditis and promote quick recovery after the illness.