Phlebitis: causes, symptoms, and effective treatment
- Understanding phlebitis: symptoms, causes, treatment
- Factors contributing to the occurrence of phlebitis
- Recognition of phlebitis symptoms
- Expert recommendations for the treatment of phlebitis
- Diagnosis of phlebitis
- Effective methods for treating phlebitis
- Prevention of phlebitis
- Interesting aspects of phlebitis
- FAQ
Understanding phlebitis: symptoms, causes, treatment
Phlebitis is an inflammatory disease of the vein walls, most often occurring as a result of thrombophlebitis. The main symptoms are pain, swelling, redness, and increased skin temperature in the area of the affected vein. The causes of phlebitis can be diverse, including prolonged standing or sitting, injuries, surgical interventions, infections, or disturbances in blood flow. Treatment of phlebitis includes wearing compression garments, taking anti-inflammatory medications, and in some cases performing surgical intervention to remove the thrombus and restore normal blood flow.
Factors contributing to the occurrence of phlebitis
Phlebitis is an inflammatory disease of the vein walls that often occurs as a result of various factors. One of the main causes of phlebitis is thrombosis – the formation of a blood clot in the venous vessels. The thrombus, in turn, can arise due to damage to the vessel wall, disruption of blood flow, or as a result of hypercoagulation.
Other factors that contribute to the development of phlebitis include infectious processes, injuries, surgical interventions, pressure sores, as well as autoimmune diseases. In some cases, phlebitis may be caused by metabolic disorders, malignant tumors, or the intake of certain medications. Understanding these factors and their impact on the development of phlebitis plays an important role in the prevention and treatment of this condition.
- Thrombosis: the formation of blood clots in the venous vessels can lead to the development of phlebitis.
- Infectious processes: the presence of infection in the body increases the risk of inflammation of the veins.
- Injuries: damage to vessels as a result of trauma can become a cause of phlebitis.
- Surgical interventions: operations on the veins or near them can provoke the development of inflammation.
- Bedsores: prolonged bed rest can cause stasis of blood flow and contribute to phlebitis.
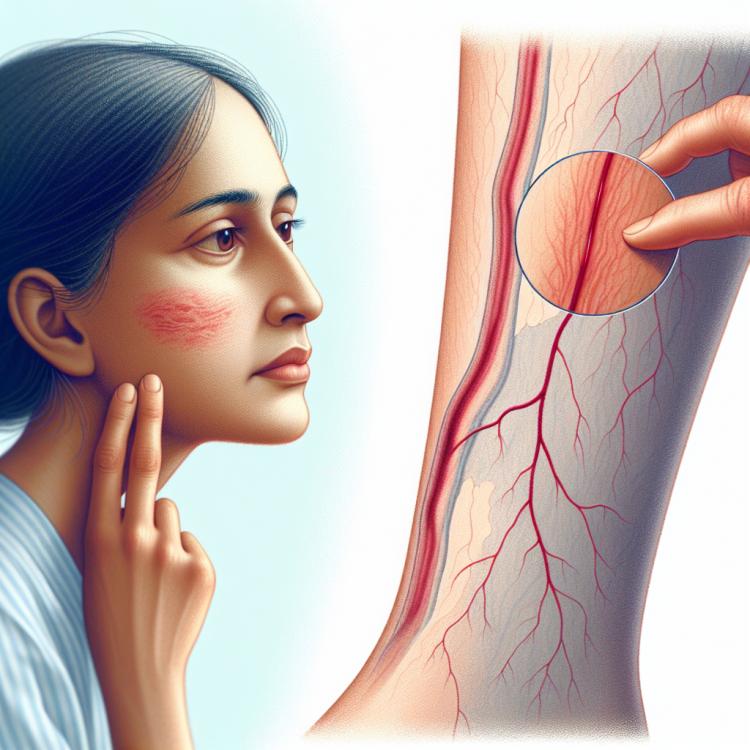
Recognition of phlebitis symptoms
Phlebitis often manifests with a variety of symptoms on the skin and venous vessels. The classic signs include pain, swelling, and redness of the skin in the area of the affected vessel. It is not uncommon to observe an increase in skin temperature around the inflamed vein.
Additional symptoms may include heaviness in the leg, itching, bruising, superficial ulcers on the skin, and changes in skin color. It is important to note that phlebitis can occur in both acute and chronic forms, therefore prompt diagnosis and treatment play a key role in preventing complications.
- Pain and discomfort: patients with phlebitis often experience pain along the inflamed vein, which may intensify upon palpation.
- Swelling and redness of the skin: swelling of the tissues and redness of the skin are often observed around the affected vessel, indicating an inflammatory response.
- Increased skin temperature: the area around the inflamed vein may feel warmer to the touch, related to vasodilation and inflammation.
- Heaviness in the leg and swelling: patients may experience a feeling of heaviness in the leg, swelling of tissues, and enlargement of the calf and foot.
- Itching and bruising: such symptoms may accompany phlebitis, indicating problems with circulation and venous outflow.
Expert recommendations for the treatment of phlebitis
Experts in the field of phlebology note that effective management of phlebitis involves a comprehensive approach. Depending on the severity of the disease and its form, conservative treatment may be applied, such as the use of anti-inflammatory drugs, pain relievers, medications to reduce swelling, and blood thinners.
However, in severe cases of phlebitis, especially with thrombosis or obvious signs of infection, surgical intervention may be required, such as sclerotherapy or surgical removal of the affected vein. Experts recommend starting treatment at the first signs of the disease, as this reduces the risk of complications and promotes the rapid recovery of the patient.

Diagnosis of phlebitis
The diagnosis of phlebitis is an important step in identifying this condition in patients. In the diagnostic process, the physician conducts a visual examination of the affected area of the skin and palpates the veins, assessing for swelling, redness, tenderness, and other characteristic signs. To confirm the diagnosis of phlebitis, additional instrumental and laboratory studies may be required, such as ultrasound examination of the veins, duplex scanning, as well as blood tests for the presence of inflammatory markers.
During the diagnosis, it is important to consider all aspects of the patient’s condition, their medical history, and to perform a differential diagnosis to exclude other diseases with similar symptoms. Accurate and timely identification of phlebitis allows for appropriate treatment to be prescribed, prevents complications, and reduces the risk of serious consequences for the patient.
- Visual inspection: the doctor conducts a detailed examination of the affected area of the skin, looking for signs of redness, swelling, and tenderness.
- Palpation of veins: palpation of the veins allows for assessing the degree of hardness, tenderness, and swelling of the affected vessel.
- Instrumental methods: ultrasound examination of the veins and duplex scanning allow for visualizing the condition of the veins and detecting possible thrombi or inflammation in the vessels.
- Laboratory studies: blood tests for inflammatory markers (such as C-reactive protein) can confirm the presence of an inflammatory process characteristic of phlebitis.
- Differential diagnosis: it is important to pay attention to symptoms similar to other diseases (such as thrombosis or lymphangitis) for an accurate diagnosis and appropriate treatment.
Effective methods for treating phlebitis
In cases of chronic phlebitis or complications related to the formation of blood clots, surgical intervention may be required. Surgical methods include sclerotherapy of the veins, thrombectomy, or phlebectomy. An individual approach to the treatment of phlebitis, taking into account the characteristics of each case, promotes effective control of the disease and prevents possible complications.
- Anti-inflammatory drugs: The use of medications aimed at reducing inflammation in the venous vessels.
- Anticoagulants: Medications that help prevent the formation of blood clots or promote their dissolution.
- Compression therapy: The use of compression bandages or stockings to improve blood flow and reduce swelling.
- Surgical methods: Surgical interventions, such as sclerotherapy, thrombectomy, or phlebectomy, may be required in complicated cases of phlebitis.
- Individual approach: Determining the most suitable treatment method depending on the type and severity of phlebitis to achieve the best outcome.
Prevention of phlebitis
An important aspect of phlebitis prevention is regular preventive examinations by a phlebologist or vascular surgeon for individuals at increased risk of developing the disease. Timely detection of the initial signs of vein inflammation and the prescription of necessary preventive and treatment measures will help maintain the normal functioning of the venous system and prevent possible complications.
- Moderate physical exercises: Regular moderate physical activities help improve blood flow and can prevent venous blood stagnation.
- Maintaining a healthy weight: Being overweight increases the load on the venous system, so controlling and maintaining a healthy weight can reduce the risk of phlebitis.
- Avoiding prolonged sitting or standing: Taking regular breaks for active movement helps maintain blood flow and prevents venous blood stasis.
- Wearing compression garments: Compression stockings or socks can improve blood flow and reduce the strain on the veins, especially in cases where prolonged sitting or standing cannot be avoided.
- Regular preventive check-ups with a specialist: Timely detection of early symptoms of phlebitis and taking appropriate measures will help prevent the progression of the disease and its complications.
Interesting aspects of phlebitis
Studying the factors that contribute to the development of phlebitis, such as blood flow disorders, infections, injuries, and others, allows for a deeper understanding of the mechanisms behind the onset and progression of this disease. Scientific research in the field of phlebitis continues to expand our knowledge of the causes, symptoms, and treatment of this condition, helping to improve prevention and therapy methods.