Frontitis: symptoms, causes, and effective treatment
- Understanding Frontitis: Symptoms, Causes, and Treatment Methods
- Factors of Frontite Development
- Clinical manifestations of frontalitis
- Expert opinions on the treatment of frontalitis
- Methods of diagnosing frontitis
- Treatment of frontal sinusitis
- Prevention of frontalitis
- Interesting aspects of frontal sinusitis
- FAQ
Understanding Frontitis: Symptoms, Causes, and Treatment Methods
Frontal sinusitis, or inflammation of the frontal sinuses, is characterized by certain symptoms such as pain in the forehead, dental arches, and eyes, nasal congestion, loss of smell, and general weakness. The causes of frontal sinusitis can be diverse, including viral or bacterial infections, allergies, and anatomical features. Treatment consists of using antibiotics for bacterial etiology, antiviral medications in the case of a viral infection, as well as symptomatic therapy to alleviate the patient’s condition.
Factors of Frontite Development
Frontitis, inflammation of the forehead sinuses, is often caused by an infection, most commonly triggered by viruses or bacteria. The development of frontitis may be associated with impaired drainage of secretions from the paranasal sinuses, leading to their filling and subsequent proliferation of microorganisms causing inflammation. However, potential causes of frontitis may also include allergies, anatomical features, and other factors that affect the condition of the sinus mucosa.
Studies show that chronic frontitis may be determined not only by an infectious nature but also have immunological, allergic, and ecological components. An important aspect is also considering risk factors, including environmental conditions, immune system status, and the presence of chronic diseases that may contribute to the development of frontitis.
- Infections: Viruses and bacteria that enter the sinuses can cause inflammation.
- Secretions drainage disorders: Impaired mucus drainage from the sinuses contributes to their filling and the development of infection.
- Allergies: The body prone to allergic reactions may be more susceptible to developing frontal sinusitis.
- Anatomical features: Certain structural characteristics of the face may make a person more prone to the development of frontal sinus inflammation.
- Risk factors: Environmental conditions, including air pollution, overall health, immune system status, and the presence of other chronic diseases, can increase the likelihood of developing chronic frontal sinusitis.
Clinical manifestations of frontalitis
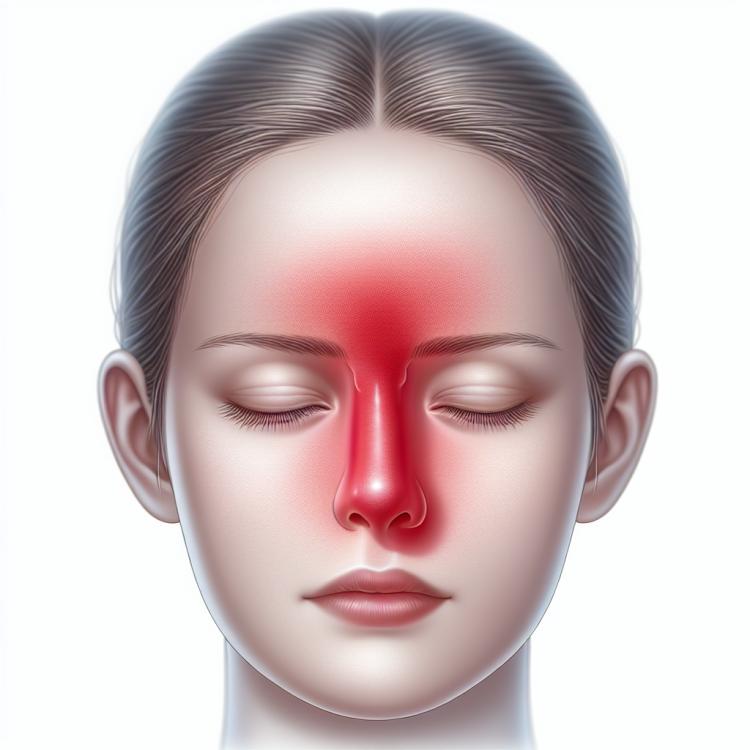
Clinical manifestations of frontal sinusitis may include symptoms typical of sinus inflammation: pain in the forehead, nose, and eyes, worsening when leaning the head, as well as a feeling of pressure in the facial area. Patients with frontal sinusitis often experience nasal congestion, smell disturbance, cough, as well as general weakness and fatigue.
More severe cases of frontal sinusitis may present with nasal discharge of pus, elevated temperature, and worsening health. For an accurate diagnosis and appropriate treatment, it is important to consult a doctor at the first signs of frontal sinusitis to prevent complications and ensure effective recovery.
- Pain and pressure in the forehead area: characteristic pain and discomfort in the forehead may be early signs of frontalitis.
- Nasal congestion: the feeling of congestion and difficulty breathing through the nose often accompanies frontalitis.
- Worsening when bending the head: intensification of symptoms when bending the head forward may indicate the possible presence of frontalitis.
- Olfactory disturbances: loss or deterioration of smell is a typical symptom of sinus inflammation, including frontalitis.
- Pus discharge from the nose: the presence of purulent discharge from the nose often indicates a more serious and prolonged sinus inflammation.
Expert opinions on the treatment of frontalitis
Experts in the field of otolaryngology recommend a comprehensive approach to the treatment of frontal sinusitis, which includes the use of antibiotics for bacterial infections, nasal drops and sprays to relieve symptoms and improve sinus drainage, as well as recommendations for humidifying the air and applying warm compresses to alleviate discomfort. In cases of chronic frontal sinusitis, additional treatment methods may often be necessary, such as physiotherapy or surgical intervention to restore normal sinus drainage.
An important aspect of treating frontal sinusitis is the individualization of the approach in each specific case, taking into account the characteristics of the disease in the particular patient. Experts emphasize the importance of following the physician’s recommendations, regularly monitoring the condition of the disease, and timely seeking medical assistance to achieve the best treatment results for frontal sinusitis and prevent possible complications.

Methods of diagnosing frontitis
The diagnosis of frontal sinusitis usually begins with a clinical examination and discussion of the symptoms with the patient. Additional diagnostic methods may include X-rays of the nasal sinuses, computed tomography (CT), or magnetic resonance imaging (MRI) for a more detailed study of the affected areas. Laboratory tests, including blood tests and nasal secretions, may also be used to identify inflammatory processes, determine the type of infection, and choose the appropriate treatment.
Effective diagnosis of frontal sinusitis plays an important role in determining the correct treatment approach and preventing complications. The combination of clinical data and the results of diagnostic procedures allows specialists to make an accurate diagnosis and develop an individual treatment plan for each patient with frontal sinusitis.
- Clinical examination: The doctor examines the patient and discusses symptoms, which helps to initiate the primary assessment of the condition.
- X-ray of the sinuses: X-ray images are used to visualize the condition of the sinuses and detect possible changes characteristic of frontal sinusitis.
- Computed tomography (CT): Allows for a more detailed study of the structure of the sinuses, revealing inflammatory changes and determining the nature of the lesion.
- Magnetic resonance imaging (MRI): Used to obtain more detailed information about the condition of the tissues and vessels of the sinuses, aiding in differential diagnosis.
- Laboratory tests: Include blood tests and nasal secretions to determine the level of inflammation, the type of infectious agent, and the body’s response to the disease.
Treatment of frontal sinusitis
To alleviate the symptoms of frontal sinusitis, local vasoconstrictor drops, anti-inflammatory medications, and nasal irrigation with saline solutions may be used. In the case of chronic frontal sinusitis, when inflammation lasts longer than 12 weeks, additional treatment methods may be required, including immune correction, surgical intervention, or other therapeutic approaches.
- Use of antibiotics: In the case of bacterial frontitis, the prescription of antibiotics may help eliminate the pathogen and get rid of the infection.
- Local vasoconstrictive drops: The use of nasal drops with vasoconstrictive action helps reduce swelling and ease breathing.
- Anti-inflammatory agents: Medications of this class help reduce inflammation in the sinuses and alleviate general symptoms of frontitis.
- Nasal irrigation: Nasal irrigation procedures using saline solutions contribute to the cleansing of the mucous membrane and reduce the accumulation of secretions.
- Surgical treatment: In cases of chronic frontitis that do not respond to conservative therapy, surgical intervention may be required to restore normal drainage function of the sinuses.
Prevention of frontalitis
Regularly rinsing the nose with saline solutions can help prevent the accumulation of secretions in the sinuses and reduce the likelihood of developing frontitis. It is also important to promptly treat respiratory infections, prevent allergic reactions, and maintain optimal humidity in indoor spaces. Following these recommendations contributes to reducing the risk of frontitis and maintaining the overall health of the nasal mucosa and sinuses.
- Strengthening the immune system: Maintain a healthy lifestyle, consume foods rich in vitamins and minerals, keep an eye on your daily routine and physical activity.
- Avoiding contact with infections: Avoid close contact with individuals suffering from respiratory infections, especially during epidemics, and follow personal hygiene rules.
- Nasal rinsing: Regularly rinsing the nose with saline solutions helps remove mucus from the sinuses and prevent their blockage.
- Effective therapy for respiratory infections: Timely consultation with a doctor and proper treatment of colds and other respiratory infections can help prevent complications, including frontal sinusitis.
- Maintaining optimal humidity in indoor spaces: Using humidifiers helps avoid dryness of the nasal mucosa, preventing irritation and increased susceptibility to infections.
Interesting aspects of frontal sinusitis
Another curious aspect of frontal sinusitis is its possible impact on overall health. Some studies indicate a potential link between chronic frontal sinusitis and other conditions, such as bronchial asthma or allergic reactions. Understanding these interconnections and searching for new methods of treatment and prevention of frontal sinusitis remain the subjects of serious scientific research.