Gastroenterocolitis in adults: diagnosis, prevention, and treatment
- Definition of gastroenterocolitis
- Factors contributing to the development of gastroenterocolitis
- Visible signs of gastroenterocolitis
- Expert opinion on methods for treating gastroenterocolitis
- Methods for diagnosing gastroenterocolitis
- Methods of treating gastroenterocolitis
- Prevention measures for gastroenterocolitis
- Amazing aspects of gastroenterocolitis
- FAQ
Definition of gastroenterocolitis
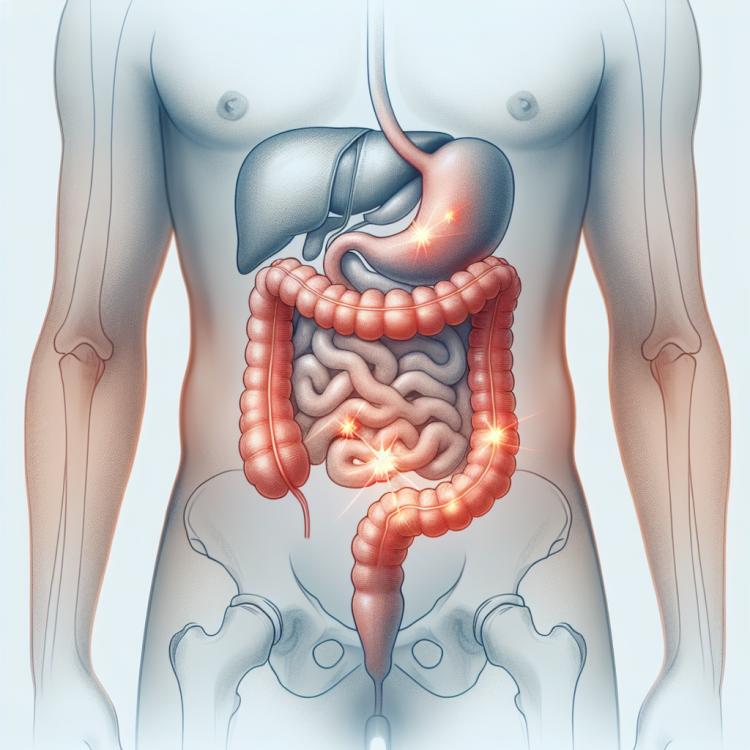
Gastroenterocolitis is an inflammatory disease that affects the mucous membrane of the stomach, intestines, and the lining of the colon. There can be various causes of gastroenterocolitis, including infections, allergic reactions, autoimmune disorders, dysbiosis, and other factors. Patients with gastroenterocolitis often experience symptoms such as abdominal pain, diarrhea, constipation, nausea, vomiting, general weakness, and other unpleasant manifestations that can significantly impact their quality of life.
Factors contributing to the development of gastroenterocolitis
Gastroenterocolitis can be caused by various factors, including infections, dysbiosis, allergic reactions, or improper nutrition. Infections are generally the most common cause of gastroenterocolitis, such as viruses, bacteria, and parasites that can cause inflammation in the gastrointestinal tract. Disruptions in the gut microbiota can also contribute to the development of gastroenterocolitis, as the balance between “good” and “bad” microorganisms can be disturbed, leading to inflammation and diarrhea.
- Infections: Viruses, bacteria, and parasites can cause inflammation in the gastrointestinal tract, contributing to the development of gastroenterocolitis.
- Dysbiosis: Disruptions in the gut microbiota can disturb the balance of microorganisms, leading to inflammation and digestive disorders.
- Allergic reactions: Food allergens or intolerance to certain products can also be factors in the development of gastroenterocolitis.
- Poor nutrition: Consuming excessive fatty or spicy foods, as well as insufficient fluid intake, can negatively affect the functioning of the gastrointestinal tract.
- Stress and psycho-emotional factors: Psychological tension and stress can worsen the symptoms of gastroenterocolitis and contribute to its development.
Visible signs of gastroenterocolitis
Gastroenterocolitis is often accompanied by a variety of symptoms, including abdominal pain, severe diarrhea, nausea, and vomiting. Abdominal pain can be cramping, spasmodic, or diffuse, and is often accompanied by abdominal bloating. Diarrhea, characterized by frequent and watery stools, may be accompanied by loss of fluids and electrolytes, which can lead to dehydration and a weakened state of the patient. Other signs may also occur, such as fever, weakness, and general malaise, depending on the severity and cause of the condition.
- Abdominal pain: pain can vary in intensity and character, including cramps, intermittent or widespread pain.
- Diarrhea: characterized by frequent and watery stools, which can lead to dehydration and loss of electrolytes.
- Nausea and vomiting: patients may experience nausea, which can be accompanied by vomiting, further increasing the risk of dehydration.
- Abdominal bloating: bloating may occur, which can cause additional discomfort for the patient.
- Fever and weakness: symptoms of gastroenterocolitis may be accompanied by an increase in body temperature, general weakness, and malaise.
Expert opinion on methods for treating gastroenterocolitis
Medical experts typically emphasize the importance of a comprehensive approach to treating gastroenterocolitis, including dietary adjustments, the use of probiotics and antibiotics in the case of infectious causes, as well as providing supportive therapy to restore the balance of intestinal microflora. They also note that when choosing treatment methods, it is essential to consider the individual characteristics of each patient and the severity of the disease.
Experts also stress that before beginning treatment for gastroenterocolitis, it is crucial to correctly diagnose its cause, as treatment methods may differ depending on the etiology of the disease. They recommend consulting a specialist for accurate diagnosis and the development of an individualized treatment plan that will be most effective and safe for each specific case of gastroenterocolitis.

Methods for diagnosing gastroenterocolitis
The diagnosis of gastroenterocolitis includes a physical examination of the patient, medical history, laboratory tests, instrumental studies, such as stool tests for hidden blood and microbiological stool analyses to identify infectious agents. Additionally, if necessary, colonoscopy and gastrofibroscopy may be used to visualize the condition of the mucous membrane of the intestines and stomach, which can help establish an accurate diagnosis and determine a treatment strategy.
- Physical examination: The doctor examines the patient, palpates the abdomen to identify tenderness and tumors, and listens for bowel sounds.
- Medical history: Gathering information about symptoms, dietary habits, medications, and other factors that may be related to the development of gastroenterocolitis.
- Stool tests: Laboratory examination to determine the presence of blood, infectious pathogens, or other abnormalities in the stool.
- Colonoscopy: An invasive procedure where the doctor uses an endoscope to examine the walls of the colon and part of the large intestine.
- Microbiological stool tests: Laboratory examination of stool to identify pathogenic microorganisms that may cause intestinal infection.
Methods of treating gastroenterocolitis
- Application of antimicrobial drugs to eliminate the pathogens of infectious gastroenterocolitis.
- Use of anti-inflammatory agents to reduce inflammation and pain syndrome in the intestines.
- Prescription of probiotics to restore healthy gut microbiota after treatment of the infectious process.
- Diet aimed at reducing the load on the digestive system and facilitating the work of the gastrointestinal tract.
- Monitoring of fluid balance and electrolytes to prevent dehydration and maintain normal body functioning.
Prevention measures for gastroenterocolitis
For the prevention of gastroenterocolitis, it is also important to pay attention to your diet by consuming food rich in fiber, vitamins, and minerals, which contributes to the healthy functioning of the intestines. Maintaining a balanced diet and avoiding excessive consumption of fatty and processed foods will help reduce the risk of developing gastroenterocolitis. Regular consumption of probiotics may also help maintain healthy intestinal microflora and reduce the likelihood of inflammatory processes.
- Observance of hygiene rules, including regular and thorough handwashing, especially before eating and after visiting public places.
- Use of only clean drinking water, avoiding potential sources of water contamination.
- Proper cooking and storage of food to prevent contamination through products.
- Regular consumption of food rich in fiber, vitamins, and minerals to maintain healthy bowel function.
- Avoidance of excessive consumption of fatty and processed foods, as well as adherence to a balanced diet.
- Regular intake of probiotics to maintain healthy gut microflora and prevent inflammatory processes.