Hemorrhoids: causes, symptoms, and effective treatment
Definition of hemorrhoids
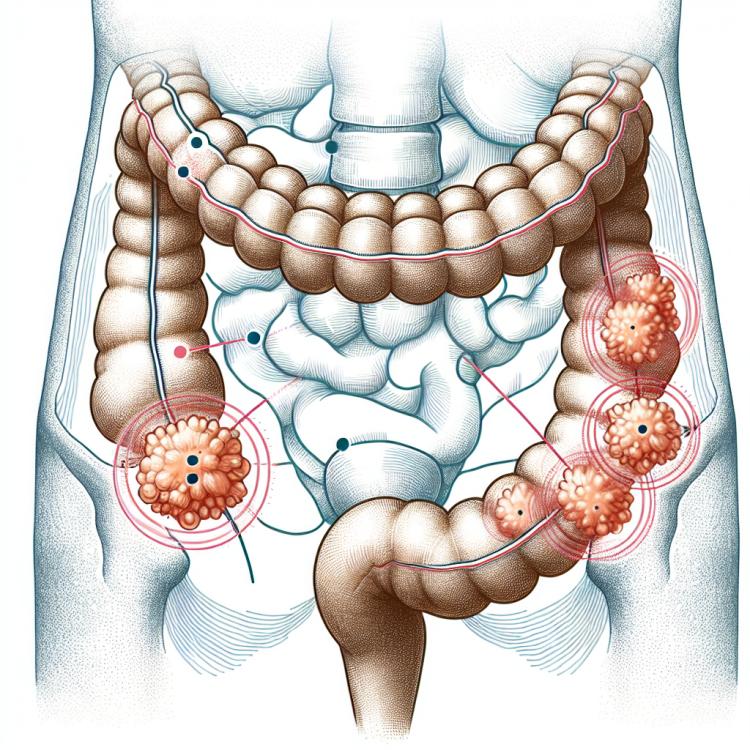
Hemorrhoids are a condition characterized by inflammation and dilation of the veins in the rectal canal and anus. Hemorrhoidal nodes can manifest as internal, located inside the rectal canal, as well as external, protruding beyond the anal opening. This is a common disease caused by blood stagnation and increased pressure in the pelvic veins, leading to the formation of nodes and various clinical manifestations, including pain, itching, bleeding, and discomfort.
Causes of hemorrhoids
Hemorrhoids, characterized by varicose veins in the rectal area, can arise from several main causes. Venous stasis caused by insufficient physical activity or prolonged sitting, as well as increased pressure in the pelvis during pregnancy or during prolonged straining during defecation, are factors that contribute to the development of hemorrhoids.
Other causes may include circulatory disorders in the pelvic veins, increased pressure from internal organs on the veins, genetic predisposition, or chronic diseases affecting the condition of the vessels. Understanding the main causes of hemorrhoids is important for preventing their occurrence and for effective treatment.
- Venous stasis: prolonged sitting or lack of physical activity can lead to slowed blood flow and increased pressure in the veins.
- Increased pressure in the pelvis: pregnancy or excessive straining during bowel movements can contribute to the development of hemorrhoids.
- Circulatory disorders in the pelvic veins: these disorders can lead to increased pressure in the venous system, worsening blood flow.
- Genetic predisposition: hereditary factors can contribute to the deterioration of vascular health and promote the development of hemorrhoids.
- Increased pressure from internal organs: conditions such as obesity or chronic diseases can exert pressure on the veins and contribute to the development of hemorrhoids.
The main symptoms of hemorrhoids
Hemorrhoids can manifest with various symptoms, ranging from mild discomfort to painful conditions. The main signs include bleeding from the rectum, itching and burning in the anal area, as well as the prolapse of nodes. Patients may experience unpleasant sensations that intensify during bowel movements or while sitting.
Other common symptoms of hemorrhoids may include inflammation and swelling of venous nodes, a feeling of incomplete bowel evacuation, and discomfort during physical activity. Different stages of hemorrhoids may be accompanied by various symptoms, and their assessment is important for accurate diagnosis and treatment planning.
- Bleeding from the rectum: blood on toilet paper or in the toilet bowl may be a sign of hemorrhoids.
- Itching and burning in the anal area: frequent sensations of itching and discomfort may indicate issues with hemorrhoidal nodes.
- Prolapse of nodes: the feeling of protrusion or sagging of tissues around the anus may be one of the symptoms of hemorrhoids.
- Unpleasant sensations during bowel movements: burning, pain, or discomfort during defecation may be related to the condition of hemorrhoids.
- Inflammation and swelling of venous nodes: nodes may increase in size, become painful, and sensitive to touch.
Expert opinion on the treatment of hemorrhoids
Experts in the field of proctology emphasize a comprehensive approach to treating hemorrhoids, which includes conservative methods, surgical interventions, and lifestyle changes. Before recommending a specific treatment, specialists conduct a detailed examination, taking into account the stage of the disease, symptoms, and the individual characteristics of the patient.
Many experts recommend starting with conservative therapy, which may include the use of medications in the form of ointments or suppositories, following dietary recommendations, and exercises to strengthen the pelvic floor muscles. However, in some cases, especially with persistent or complicated forms of hemorrhoids, surgical treatment may be necessary to achieve the best results and prevent potential complications.

Hemorrhoid diagnosis
When diagnosing hemorrhoids, the doctor typically conducts a medical history, including studying symptoms, and inspects the rectal area using visual examination methods or instrumental methods such as anoscopy or rectoscopy. It is important to identify the characteristic signs of hemorrhoidal nodes, the degree of their prolapse, the presence of bleeding, as well as to assess the overall condition of the blood vessels and tissues.
To confirm the diagnosis of hemorrhoids, additional methods such as colonoscopy or recto-sigmoidoscopy may be used to rule out other diseases of the rectum. Accurate diagnosis allows for the determination of the stage of hemorrhoids, the selection of the most effective treatment method, and the prevention of complications.
- Anamnesis and symptoms: studying patient complaints and characteristic signs of hemorrhoids.
- Visual examination: examination of the rectal area to identify hemorrhoidal nodes and assess their condition.
- Instrumental methods: performing anoscopy or rectoscopy for detailed study of the blood vessels and tissues of the rectum.
- Additional studies: colonoscopy or recto-sigmoidoscopy to exclude other intestinal diseases.
- Assessment of the degree of hemorrhoids: determining the stage of the disease and choosing the most appropriate treatment method.
Treatment of hemorrhoids
The goal of hemorrhoid treatment is to relieve symptoms, prevent complications, reduce the risk of recurrence, and improve the patient’s quality of life. An individual approach to selecting treatment methods, taking into account the stage of hemorrhoids, the presence of complications, and the characteristics of the patient’s body, allows for achieving the best results and improving the prognosis of the disease.
- Lifestyle changes: includes increasing physical activity, a rich diet, weight management, and avoiding prolonged sitting.
- Medication use: use of medications to improve blood flow, reduce inflammation, promote wound healing, and ease defecation.
- Local treatment: application of ointments, creams, suppositories, or gels to relieve hemorrhoid symptoms.
- Minimally invasive procedures: performing procedures such as sclerotherapy, laser coagulation, or rubber band ligation to reduce the size and prolapse of hemorrhoids.
- Surgical treatment: intervention in the form of hemorrhoidectomy or ligation of hemorrhoids may be required in cases of advanced or complicated forms of hemorrhoids.
Prevention of hemorrhoids
Other important aspects of prevention include avoiding prolonged straining during defecation, regular water intake to prevent constipation, as well as leading an active lifestyle. Following these recommendations helps reduce the risk of developing hemorrhoids and supports the health of the rectum.
- Fiber-rich diet: Consuming enough fiber helps maintain normal intestinal peristalsis, preventing constipation.
- Maintaining optimal weight: Excess weight can increase pressure in the abdominal cavity, which contributes to the development of hemorrhoids.
- Active lifestyle: Regular physical exercise promotes better circulation and overall body condition.
- Avoiding prolonged sitting: Frequent changes in body position and leg exercises can help prevent blood stagnation in the pelvic veins.
- Regular fluid intake: Drinking enough water daily helps prevent constipation and maintain optimal bowel function.
Interesting facts about hemorrhoids
Another interesting fact about hemorrhoids is their connection to a sedentary lifestyle and lack of physical activity. Regular physical exercise and proper nutrition can help prevent or alleviate the symptoms of hemorrhoids, highlighting the importance of a healthy lifestyle for maintaining rectal health.