Endometrial hypoplasia: symptoms, diagnosis, and modern treatment methods
- Understanding Endometrial Hypoplasia: Key Aspects and Definition
- Factors contributing to endometrial hypoplasia
- Possible manifestations of endometrial hypoplasia
- Experts’ opinions on the treatment methods for endometrial hypoplasia
- The main methods for diagnosing endometrial hypoplasia.
- Methods for treating endometrial hypoplasia
- Measures to prevent endometrial hypoplasia
- Amazing aspects and facts about endometrial hypoplasia
- FAQ
Understanding Endometrial Hypoplasia: Key Aspects and Definition
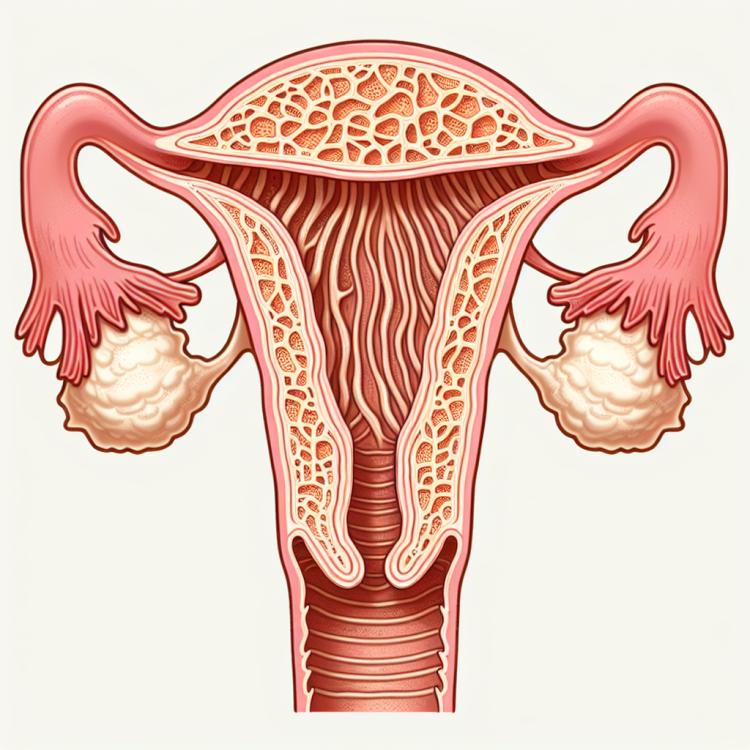
Endometrial hypoplasia is a condition characterized by insufficient development of the uterine mucosa, which plays a crucial role in the implantation of a fertilized egg. This pathological process can lead to infertility and other disorders in the conception process. Important aspects of understanding endometrial hypoplasia include early diagnosis using modern examination methods and the appointment of treatment aimed at normalizing the development of the endometrium to increase the chances of successful pregnancy.
Factors contributing to endometrial hypoplasia
Endometrial hypoplasia can be caused by a variety of factors, including genetic anomalies, hormonal imbalances, inflammatory processes, and damage such as previous surgical interventions in the area of the uterus or trauma. Other causes may include prolonged use of certain medications, possible endocrine disorders, and environmental factors such as radiation. Understanding these factors is crucial for the diagnosis and treatment of endometrial hypoplasia, as it allows for a more personalized approach to managing this condition.
- Genetic anomalies: the presence of hereditary mutations may affect the development of the endometrium.
- Hormonal imbalances: changes in the hormonal background of the body can impact the formation and restoration of the endometrium.
- Inflammatory processes: chronic inflammation in the area of the uterus can reduce the endometrium’s ability to regenerate normally.
- Surgical interventions: surgeries on the uterus or other damage in this area can affect the condition of the endometrium.
- Prolonged use of medications: the use of certain medications, especially hormonal ones, can influence the tissue of the endometrium.
Possible manifestations of endometrial hypoplasia
Symptoms of endometrial hypoplasia may include irregular or heavy menstrual bleeding, painful menstruation, undifferentiated vaginal discharge, abnormal ultrasound findings of the uterus. Women with this condition may also experience infertility and issues with conception and carrying a pregnancy, which may be associated with changes in the structure and function of the endometrium. At the first signs of a possible structural disruption of the endometrium, it is recommended to consult a doctor for diagnosis and appropriate treatment.
- Irregular or heavy menstrual bleeding: deviations from the typical menstrual cycle may be predictive symptoms of endometrial hypoplasia.
- Menstrual pain: pain during or before menstruation may be one of the manifestations of this condition.
- Undifferentiated discharge from the genital tract: changes in the type of discharge may be related to endometrial hypoplasia.
- Abnormal ultrasound findings of the uterus: images of the uterine cavity that differ from the norm in ultrasound diagnostics may indicate endometrial hypoplasia.
- Infertility and problems with conception and carrying a pregnancy: endometrial hypoplasia can be one of the causes of reproductive disorders in women.
Experts’ opinions on the treatment methods for endometrial hypoplasia
Experts in the field of gynecology recommend a comprehensive approach to treating endometrial hypoplasia, which includes medication therapy, surgical methods when necessary, and the use of modern techniques for endometrial restoration. Pharmacological treatment may include hormonal preparations to stimulate the growth of the uterine lining, as well as the use of vasodilators to improve blood supply to the endometrium.
However, when choosing a treatment method, specialists also consider the individual characteristics of each patient, her age, and health condition in order to achieve optimal results and minimize the risks of potential complications. The expert opinion emphasizes the importance of timely diagnosis and individualized treatment to achieve effective results in the fight against endometrial hypoplasia.

The main methods for diagnosing endometrial hypoplasia.
Diagnosis of endometrial hypoplasia usually includes a clinical examination by a specialist, patient history, discussion of symptoms and complaints. To confirm the diagnosis, additional examinations are often conducted, such as ultrasound of the uterus, hysteroscopy, combined histological and hormonal analyses. The effectiveness of diagnosing endometrial hypoplasia largely depends on the accuracy and scope of the studies performed, which helps specialists choose the optimal treatment plan for each specific case.
- Clinical examination: the doctor performs an examination and talks with the patient about possible symptoms, the history of the disease, and the general condition.
- Ultrasound examination of the uterus: conducting ultrasound scanning can help identify changes in the structure and thickness of the endometrium.
- Hysteroscopy: the use of a hysteroscope allows for direct visualization of the inner surface of the uterus for detailed study and tissue sampling.
- Histological analysis: analysis of tissue samples taken during hysteroscopy or other procedures can help clarify the diagnosis and determine structural changes.
- Hormonal analysis: measuring the levels of certain hormones, such as estrogens and progesterone, can provide information about the hormonal background and possible imbalances.
Methods for treating endometrial hypoplasia
- Hormonal therapy: The use of hormonal medications to correct hormonal levels and stimulate the growth of the endometrium.
- Surgical treatment: Possible surgeries to restore the endometrium and correct areas of hypoplasia.
- Embryo implantation: The use of the embryo implantation method in the uterus for patients planning a pregnancy.
- Hormone replacement therapy: The use of hormonal medications to regulate the hormonal status in the body.
- Modern treatment methods: Include innovative techniques such as growth factor therapy, stem cells, or activation of reparative processes in tissues.
Measures to prevent endometrial hypoplasia
- Maintaining hormonal balance: Regular adherence to the timeline for taking hormonal medications prescribed by a gynecologist.
- Moderate physical activity: Regular exercise contributes to improved overall health and the functioning of the reproductive system.
- Healthy nutrition: A diet rich in vitamins, minerals, and nutrients helps maintain health and normal endometrial function.
- Avoiding bad habits: Quitting smoking, moderate alcohol consumption, and avoiding narcotics reduce the risk of reproductive system diseases.
- Regular preventive check-ups: Visiting a gynecologist for a preventive examination and monitoring the condition of the endometrium.
Amazing aspects and facts about endometrial hypoplasia
The study of endometrial hypoplasia also emphasizes the importance of regular medical monitoring and control over the state of the reproductive system. Prevention and timely detection of endometrial hypoplasia can help improve the quality of life for women by preventing or minimizing the negative consequences of this condition.