Hypovolemic shock: mechanism, diagnosis, and treatment
- Basics of hypovolemic shock
- Etiology of hypovolemic shock
- The clinical picture of hypovolemic shock
- Expert opinion on the treatment of hypovolemic shock
- Methods for diagnosing hypovolemic shock
- Effective methods for treating hypovolemic shock
- Measures to prevent hypovolemic shock
- Amazing facts about hypovolemic shock
- FAQ
Basics of hypovolemic shock
Hypovolemic shock is a severe condition caused by a significant decrease in the volume of circulating blood in the body. This leads to impaired blood supply to organs and tissues, which can result in serious complications, including organ failure and death. Effective treatment of hypovolemic shock includes restoring blood volume, maintaining hemodynamic stability, and early stabilization of the patient’s condition to prevent severe complications.
Etiology of hypovolemic shock
Hypovolemic shock occurs due to significant loss of fluid from circulation, disturbances in the volume of circulating blood, or insufficient return of venous blood to the heart. The causes can be diverse, including excessive blood loss from injuries, burns, bleeding, as well as heavy sweating due to dehydration or vomiting. It is important to consider that hypovolemic shock can also be a consequence of severe dehydration and redistribution of fluids in the body, accompanying various conditions and diseases.
- Bleeding: acute or chronic bleeding, including internal and external, can lead to significant blood volume loss.
- Injuries: severe injuries, such as accidents or surgeries, can cause critical fluid loss from the body.
- Burns: burns of varying degrees can lead to significant dehydration and fluid loss through damaged skin.
- Excessive sweating: prolonged excessive sweating in high temperatures or while taking certain medications can lead to dehydration and the development of shock.
- Vomiting and diarrhea: excessive vomiting or diarrhea can lead to a large loss of fluids and electrolytes, contributing to the development of hypovolemic shock.
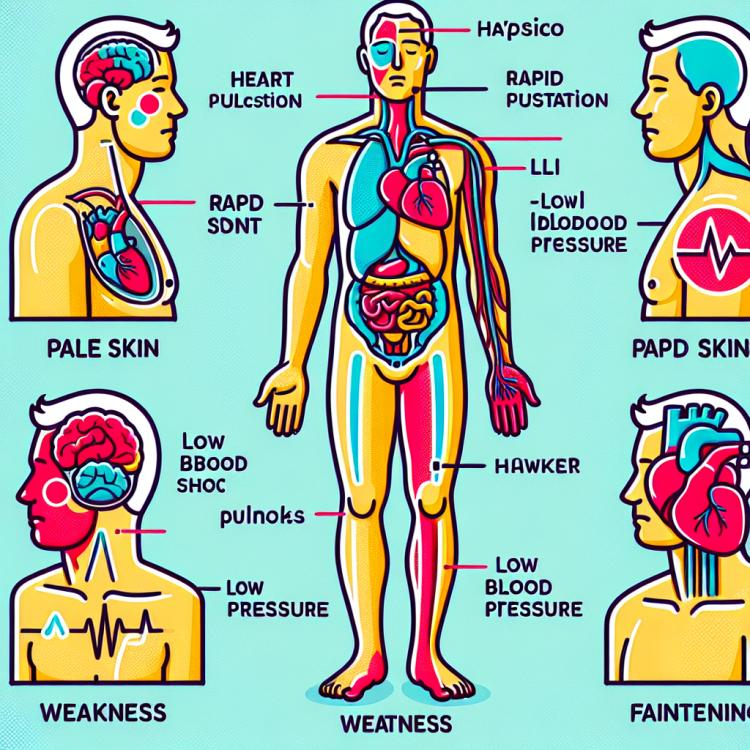
The clinical picture of hypovolemic shock
The clinical picture of hypovolemic shock is usually characterized by various symptoms, including reduced blood pressure, tachycardia, pale skin, cold sweat, chills, weakness, drowsiness, a shift in pulse pressure to lower values, and disturbances of consciousness in severe cases. Patients may experience dizziness, a sense of disorientation, or even loss of consciousness due to a lack of oxygen and nutrients reaching the brain. It is important to note that in the case of hypovolemic shock, symptoms can rapidly progress, and emergency medical assistance is necessary to prevent serious complications.
- Low blood pressure: acute blood volume loss leads to a drop in blood pressure, which is one of the characteristic signs of hypovolemic shock.
- Tachycardia: an increase in heart rate is the body’s compensatory response to a decrease in circulating blood volume.
- Pallor of the skin: due to reduced blood supply to organs and tissues, the skin may become pale and cold.
- Cold sweat: manifests as a result of peripheral vasoconstriction, when the body tries to retain heat by constricting skin capillaries.
- Consciousness disturbances: in severe cases of hypovolemic shock, symptoms of disorientation, drowsiness, dizziness, and even loss of consciousness may occur.
Expert opinion on the treatment of hypovolemic shock
Experts in the field of medicine agree on the importance of a timely and comprehensive approach to the treatment of hypovolemic shock. The main areas of therapy include restoring circulating blood volume, controlling hemodynamics, eliminating the causes of fluid loss, maintaining blood pressure, and ensuring adequate blood flow to organs and tissues. At the same time, it is necessary to take into account the individual characteristics of the patient, the presence of comorbidities, and the degree of shock severity.
Experts also emphasize the importance of monitoring hemodynamic indicators, including blood pressure, heart rate, central venous pressure, blood lactate levels, and other parameters. The main principles of treating hypovolemic shock include early diagnosis, rapid resuscitation, effective restoration of circulating blood volume, elimination of the causes of shock, and prevention of potential complications.

Methods for diagnosing hypovolemic shock
To identify hypovolemic shock, it is important to conduct a comprehensive examination of the patient, including measuring blood pressure, pulse, respiratory rate, assessing skin color, checking the condition of mucous membranes, and identifying other characteristic signs. Additional diagnostic methods include laboratory tests, such as blood tests for hemoglobin, hematocrit, electrolytes, as well as assessing lactate levels, which allows for further evaluation of the degree of tissue hypoxia and metabolic disorders.
Instrumental diagnostic methods, such as ultrasound (ultrasound of the abdominal cavity, heart), X-ray, and computed tomography, can also be used to rule out other conditions and clarify the diagnosis. Timely and accurate diagnosis of hypovolemic shock plays a key role in selecting the appropriate therapy and improving the prognosis for the patient.
- Clinical examination: includes measuring blood pressure, pulse, respiratory rate, assessing skin color, the condition of mucous membranes, and other characteristic signs.
- Laboratory tests: include blood tests for hemoglobin, hematocrit, electrolytes, assessment of lactate levels, and other indicators for additional evaluation of tissue hypoxia and metabolic disorders.
- Instrumental methods: include ultrasound examination of the abdominal cavity and heart, radiography, and computed tomography for clarifying the diagnosis and ruling out other conditions.
- Measurement of lactate levels: a marker of tissue hypoxia and perfusion, which can help in assessing the severity of the condition and planning treatment.
- Assessment of fluid balance and total circulating blood volume: important components in the diagnosis of hypovolemic shock to check the impact of fluid loss on the body.
Effective methods for treating hypovolemic shock
Additional measures include ensuring adequate oxygenation usually through oxygen therapy, correcting acidosis, monitoring electrolyte balance, and addressing the underlying condition that led to the development of hypovolemic shock. An individualized approach to treatment is critical, taking into account the specifics of each particular case and supporting the vital organs of the patient.
- Restoration of circulating blood volume: infusions of saline and colloid solutions to restore fluid and blood volume.
- Use of vasopressors: if necessary, used to maintain arterial pressure and improve hemodynamics.
- Oxygen therapy: ensuring adequate oxygenation of organs and tissues through oxygen therapy.
- Correction of acidosis: regulating acid-base balance to improve tissue oxygen exchange.
- Monitoring electrolyte balance: maintaining optimal electrolyte levels in the body to prevent complications.
Measures to prevent hypovolemic shock
Training medical staff and patients about the early signs of hypovolemic shock and methods to prevent blood loss also plays a crucial role in prevention. Proactive management of the patient’s condition, optimization of circulating blood volume, and moderate fluid therapy help reduce the risk of developing hypovolemic shock and improve treatment outcomes.
- Early diagnosis and treatment of potential causes: Timely identify and eliminate conditions that may lead to fluid loss, such as injuries, bleeding, or dehydration.
- Monitoring hemodynamic status: Maintain stable blood pressure and effective organ perfusion to prevent the development of shock.
- Training of medical personnel and patients: Clarify early signs of hypovolemic shock and methods to prevent blood loss, especially in cases of increased risk.
- Optimization of circulating blood volume: A proactive approach to managing patient condition, especially in cases of trauma or surgery, aimed at preventing the development of shock.
- Moderate fluid therapy: Proper use of fluid infusions to maintain optimal circulating blood volume and prevent the body’s decompensation.
Amazing facts about hypovolemic shock
Another interesting fact is that hypovolemic shock can manifest with various specific symptoms, including low blood pressure, tachycardia, pale skin, dizziness, and weakness. These signs may be the first signals that the body is experiencing serious disturbances due to loss of fluid and circulating blood. Familiarity with these facts helps to understand the importance of timely diagnosis and treatment of hypovolemic shock to preserve the patient’s health.