Purulent periostitis: causes, symptoms, and treatment methods
- Definition of purulent periostitis
- Etiology of purulent periostitis
- The clinical picture of purulent periostitis
- The specialists’ view on the treatment methods for purulent periostitis
- Methods for diagnosing purulent periostitis
- Methods for treating purulent periostitis
- Prevention measures for purulent periostitis
- Fascinating aspects of purulent periostitis
- FAQ
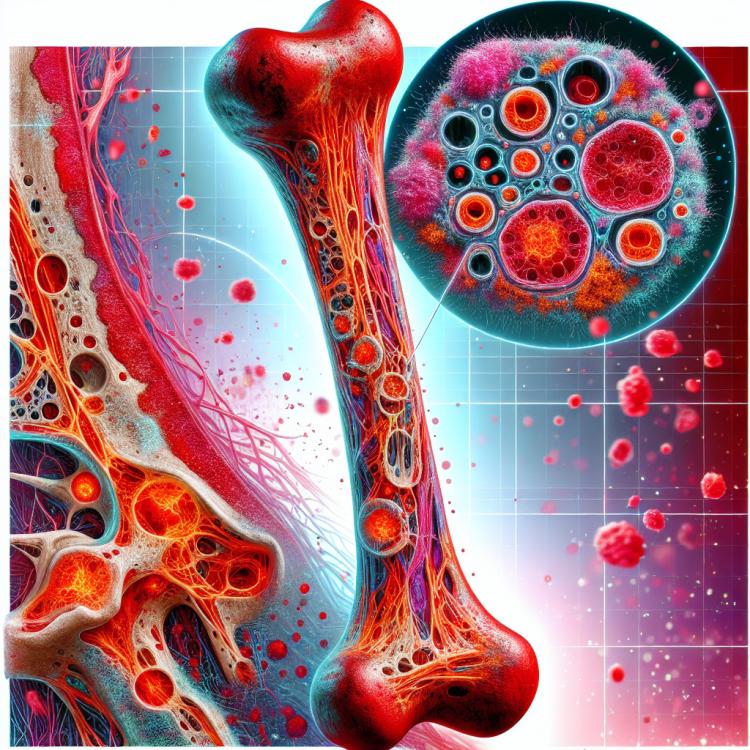
Definition of purulent periostitis
Purulent periostitis is an inflammatory disease characterized by the damage to the periosteum of the bones in the body. The primary cause of purulent periostitis is an infection that can penetrate the tissues through wounds, injuries, or the bloodstream. As a result, the infection leads to the proliferation of pathogens in the periosteum, causing inflammation, swelling, and purulent discharge, which results in characteristic symptoms and complications for the patient.
Etiology of purulent periostitis
Purulent periostitis usually occurs as a result of an infectious process when bacteria penetrate the bone marrow through locally affected dermis or soft tissues. The main pathogens may include staphylococci, streptococci, or other infectious agents. The causes of purulent periostitis may also include weakening of the immune system, injuries, or surgical interventions that contribute to infection and the development of inflammation in the bone tissue.
Other factors influencing the occurrence of purulent periostitis may include systemic infections, poor blood supply to the bone, metabolic disorders, the use of immunosuppressants or chemotherapy, which leads to a disruption of the body’s protective mechanisms and increases the risk of developing infectious complications in the bones and joints.
- Infectious process: bacteria are introduced into the bone marrow through affected dermis or soft tissues.
- Pathogens: the main bacterial agents are staphylococci and streptococci.
- Immunosuppression: reduced immunity may contribute to the development of infection in the bones.
- Injuries or surgical interventions: open wounds and surgeries can increase the risk of bone infection.
- Systemic infections: the presence of infections in other organs may increase the likelihood of developing purulent periostitis.
The clinical picture of purulent periostitis
The clinical picture of purulent periostitis may include local signs of inflammation, such as swelling, redness, tenderness, and increased temperature in the area of the affected bone. Patients may also experience increasing pain and limited mobility in the affected area. In cases where the infection is not controlled or progresses, general symptoms of intoxication may arise, such as fever, weakness, nausea, and vomiting, which require immediate medical intervention.
- Local signs of inflammation: They are characterized by swelling, redness, and increased temperature in the affected bone area.
- Pain and limited mobility: Patients may experience worsening pain and difficulty in movement in the affected area.
- General symptoms of intoxication: They may include fever, weakness, nausea, and vomiting, especially with the progression of the infection.
- Consequences of inadequate treatment: Ineffective or absent treatment of purulent periostitis can lead to complications such as sepsis or even abscesses in the soft tissues.
- Medical diagnosis: The diagnosis of purulent periostitis is based on clinical manifestations, history data, and results of laboratory and instrumental studies.
The specialists’ view on the treatment methods for purulent periostitis
Experts in the field of medicine emphasize the importance of a comprehensive approach to the treatment of purulent periostitis, which includes antibiotic therapy to combat infection, drainage of the purulent focus to eliminate the accumulation of pus, as well as maintaining adequate pain relief and rehabilitation of the affected area. The effectiveness of treating purulent periostitis depends on timely diagnosis and the prescription of adequate therapy, taking into account the sensitivity of pathogens to antibiotics and the individual characteristics of the patient.
Modern technologies in surgery also play a significant role in the treatment of purulent periostitis. Experts note considerable advancements in the use of minimally invasive methods for draining the purulent focus, which helps to speed up recovery and reduce the risk of complications. A comprehensive intervention involving specialists from various medical fields, such as surgeons, infectious disease specialists, and rehabilitation therapists, is essential for the effective treatment of purulent periostitis and the prevention of disease recurrences.

Methods for diagnosing purulent periostitis
For the diagnosis of purulent periostitis, various methods are used, including clinical examination and history taking, laboratory, and instrumental studies. The doctor conducts a physical examination to identify signs of inflammation in the affected bone area, such as swelling, redness, and tenderness. Laboratory tests, such as blood tests for inflammatory markers and blood cultures to identify infectious agents, can also assist in establishing the diagnosis of purulent periostitis.
Instrumental diagnostic methods include X-rays, computed tomography (CT), and magnetic resonance imaging (MRI). X-rays can show changes in the bone, such as periosteal reaction or destruction of bone tissue. Computed and magnetic resonance imaging provide more detailed information about the condition of the bones, joints, soft tissues, and adjacent structures, helping to clarify the diagnosis and treatment plan.
- Clinical examination and history: The doctor conducts a visual examination to identify signs of inflammation in the affected bone area and gathers information about symptoms from the patient.
- Laboratory tests: Blood may be analyzed for inflammatory markers, such as elevated levels of C-reactive protein (CRP) or leukocytes, and a blood culture may be taken to identify infectious agents.
- X-ray: This method can be used to visualize changes in the bone, such as periosteal reaction, bone tissue destruction, or purulent collections.
- Computed tomography (CT): CT provides a more detailed image of the condition of the bone and surrounding tissues, which can help clarify the diagnosis and plan treatment.
- Magnetic resonance imaging (MRI): MRI can be used for a more detailed study of the bone, joints, soft tissues, and adjacent structures, providing additional information for diagnosing purulent periostitis.
Methods for treating purulent periostitis
In cases of severe pain and inflammation, anti-inflammatory drugs or analgesics may be prescribed to patients. Physical therapy may also be used to improve blood circulation in the affected area and strengthen tissues during the rehabilitation process after treatment. Proper and timely treatment of purulent periostitis not only contributes to the resolution of the infection but also reduces the risk of complications and improves the prognosis of the disease.
- Antibiotic therapy: Treatment of purulent periostitis often includes the use of antibiotics to combat infection and prevent its spread. To optimally select an antibiotic, it is necessary to know the type of pathogen and the results of cultures for antibiotic sensitivity.
- Surgical intervention: In cases of complications or lack of improvement due to conservative treatment, surgical drainage of the purulent focus or removal of affected tissues may be required.
- Anti-inflammatory medications and analgesics: For severe pain and inflammation, medications may be prescribed to relieve pain and reduce the inflammatory process.
- Physiotherapy: Physiotherapeutic procedures may be used to improve blood circulation in the affected area, reduce pain, and strengthen tissues during the recovery process after treatment.
- Regular monitoring and control: It is important to conduct constant monitoring of the patient’s condition, the dynamics of the disease, and the results of treatment to timely adjust therapy and prevent complications.
Prevention measures for purulent periostitis
A healthy lifestyle, including balanced nutrition, exercises to maintain bone mass, and support for the immune system, can also contribute to strengthening the body and reducing the risk of infections, including purulent periostitis. It is important to pay attention to essential nutrients, including calcium and vitamin D, to maintain bone health and adhere to recommendations for the prevention of injuries and infections.
- Maintaining skin and wound hygiene: Regular washing and treatment of damaged areas of the skin helps prevent bacteria from entering the body through the skin.
- Timely consultation with a doctor: In the presence of bone injuries or signs of inflammation in the area of the bones, it is important to promptly consult a specialist for diagnosis and treatment of infections.
- Adhering to a healthy lifestyle: A healthy diet, regular exercise, maintaining the immune system, and strengthening bone mass contribute to strengthening the body and reducing the likelihood of infections.
- Calcium and vitamin D-rich nutrition: Consuming foods that contain sufficient amounts of calcium and vitamin D helps maintain bone health and reduce the risk of injuries and infections.
- Avoiding injuries and fractures: Preventing injuries and fractures, especially in more vulnerable population groups, is an important aspect of the prevention of purulent periostitis.
Fascinating aspects of purulent periostitis
An interesting aspect of purulent periostitis is its variable clinical picture, which can pose a challenge for accurate diagnosis. In addition, various factors, such as the causative agents of the infection, the state of the immune system, and the presence of systemic diseases, can influence the development and course of this condition, making its study interesting for medical professionals.