Hiatal hernia: everything you need to know
Understanding a hiatal hernia
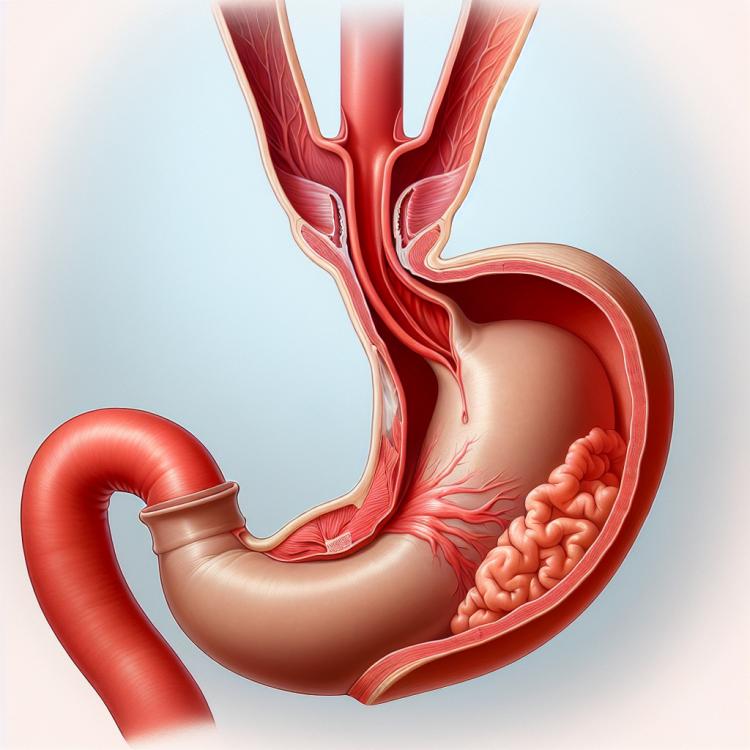
A hiatal hernia (HH) is a condition where the upper part of the stomach pushes through the diaphragm at the esophageal opening. This can lead to various symptoms, including heartburn, difficulty swallowing, nausea, and chest pain. Chronic hiatal hernia can lead to complications such as esophagitis or bleeding.
Diagnosis of hiatal hernia usually involves endoscopy, X-ray, or computed tomography (CT scan). Treatment for this condition may include dietary changes, lifestyle modifications, medications to reduce heartburn, or, in some cases, surgery to restore the anatomical integrity of the diaphragm’s esophageal opening.
Etiology of hiatal hernia
A hiatal hernia, also known as esophageal hernia disorder, occurs due to weakness or defect in the diaphragmatic opening through which the esophagus passes. The main causes of a hiatal hernia include weakening of the ligaments and muscles of the diaphragm, which may be due to factors such as age, obesity, pregnancy, as well as increased pressure in the abdominal cavity.
Other factors contributing to the development of a hiatal hernia include disruptions in the normal functioning of the diaphragm, any injuries, or heavy physical stress. As a result of the compression of the esophagus and part of the stomach through the opening in the diaphragm, a hiatal hernia can cause a number of unpleasant symptoms and requires timely medical attention for accurate diagnosis and determination of optimal treatment.
- Weakening of diaphragm ligaments and muscles: age, obesity, pregnancy, and increased pressure in the abdominal cavity can lead to a decrease in the tone of the diaphragm muscles.
- Disorders in diaphragm function: defects or damage in the diaphragm can contribute to the development of a hiatal hernia.
- Injuries: sustained injuries, especially in the abdominal area, can be a factor contributing to the early development of a hernia.
- Heavy physical exertion: excessive pressure in the abdominal cavity associated with lifting heavy objects or other forms of physical activity can increase the risk of hernia development.
- Hereditary factors: genetic traits may play a role in the occurrence of hiatal hernias in some individuals.
The clinical picture of a hiatal hernia
A diaphragmatic hiatal hernia can manifest with various symptoms, including heartburn, a feeling of heaviness in the abdomen after eating, belching, frequent vomiting, epigastric pain, and difficulty swallowing. Patients may also experience respiratory issues, such as cough, shortness of breath, and wheezing, caused by the reflux of stomach contents into the esophagus.
More severe symptoms of a hiatal hernia can include coughing up blood, black or bloody stools, which may indicate developing complications such as perforation or bleeding. If the mentioned signs appear, it is important to consult a doctor for diagnosis and establishing an accurate diagnosis, as timely treatment can prevent serious complications and improve the prognosis of the disease.
- Heartburn: a burning sensation in the chest that may worsen after eating.
- Heaviness in the abdomen: a feeling of pressure or discomfort in the upper abdomen, especially after eating.
- Belching: an unpleasant sensation of food or liquid returning from the stomach to the esophagus.
- Epigastric pain: painful sensations in the area of the abdomen between the sternum and the navel.
- Difficulties swallowing: the sensation of food getting stuck in the esophagus or difficulties in swallowing.
Expert opinion on the treatment of hiatal hernia
Experts in the field of gastroenterology identify several treatment methods for hiatal hernia, depending on the severity of the case and the presence of complications. One of the main treatment methods is conservative therapy, which includes dietary changes, the use of medications that reduce gastric acidity, as well as alleviating symptoms of heartburn. Effective measures also include weight reduction in cases of obesity, controlling intra-abdominal pressure, and avoiding factors that exacerbate the disorder.
In cases where conservative methods do not yield the desired results or complications are present, surgical intervention may be necessary. Surgical correction of hiatal hernia can include various methods such as lower esophagectomy, Nissen fundoplication, or laparoscopic gastroesophagectomy, depending on the individual characteristics of the patient and the recommendations of the medical specialist.

Examination of hiatal hernia
Diagnosis of hiatal hernia is conducted using various methods, including esophagostopronosonography (ESG), X-ray, computed tomography (CT), and MRI of the chest. ESG is an important method for diagnosing hiatal hernia, allowing for real-time visualization of the esophagus and stomach and detecting the presence of a hernia. X-ray can also be used to diagnose this condition, sometimes with the application of a contrast agent for a more detailed examination of the area.
Additionally, to clarify the diagnosis and identify complications, endoscopy of the esophagus, stomach, and intestines may be required. Accurate and timely diagnosis of hiatal hernia plays a crucial role in determining the causes of symptoms and choosing the most effective treatment for the patient.
- Esophagostopronosonography (ESG): A method that allows visualizing the condition of the esophagus and stomach in real time to detect a hiatal hernia.
- X-ray: Used for diagnosing a hiatal hernia, often with the application of a contrast agent for a more detailed examination of the area.
- Computed tomography (CT): An educational diagnostic method that helps identify the presence of a hernia and assess its characteristics and degree of development.
- Magnetic resonance imaging (MRI) of the chest: Used to obtain detailed images of pathological changes in the area of the hiatal hernia.
- Endoscopy of the esophagus, stomach, and intestines: A method that may be required to clarify the diagnosis and identify complications in the case of a hiatal hernia.
Strategies for treating hiatal hernia
In cases where conservative methods do not provide improvement and the level of discomfort remains significant, surgical intervention may be necessary. Surgical correction of hiatal hernia may involve various surgical techniques, such as laparoscopic Nissen fundoplication or medial repair of the diaphragm opening, aimed at returning the esophagus and upper part of the stomach to their proper position and restoring normal anatomy.
- Lifestyle changes: includes quitting smoking, limiting alcohol consumption, controlling weight, and eliminating factors that contribute to increased pressure in the abdominal cavity.
- Diet: it is recommended to follow a diet aimed at reducing gastric acid reflux, including avoiding spicy, fatty foods, chocolate, coffee, and citrus fruits.
- Exercises to strengthen abdominal muscles: specialized exercises can help strengthen the abdominal muscles and improve diaphragm support.
- Medication therapy: prescription of medications to reduce gastric acidity and symptomatic treatment, such as antiemetics.
- Surgical intervention: in cases where conservative methods are ineffective, surgical correction may be required, such as laparoscopic fundoplication or medial repair of the diaphragm hole.
Preventive measures for hiatal hernia
Additionally, avoiding lifting heavy objects, especially with improper lifting techniques, as well as avoiding overeating and consuming food before bedtime can contribute to lowering the risk of developing a hernia. Patients with risk factors for this condition, such as obesity or diseases, should be regularly examined by a doctor and follow preventive recommendations to avoid complications.
- Maintaining a healthy weight: Regular physical exercise and healthy eating help reduce pressure in the abdominal cavity and decrease the risk of hernia.
- Limiting the intake of fatty foods: Avoiding excessively fatty and heavy foods can help prevent excessive pressure in the abdomen, which may contribute to the development of a hernia.
- Avoiding heavy lifting: Incorrectly lifting heavy objects can increase pressure in the abdominal cavity, so it is important to avoid unnecessary strain when lifting items.
- Regular check-ups with a doctor: Patients with risk factors should see a doctor regularly for timely diagnosis and monitoring of the esophagus and diaphragm condition.
- Careful eating before bedtime: Avoiding excessive food intake before sleep can help prevent undue pressure on the diaphragm during nighttime rest.