Schmorl’s Node: manifestations, diagnosis, and treatment options
- Understanding Schmorl’s Hernia: Essence and Features
- Etiology of Schmorl’s Hernia
- The clinical picture of Schmorl’s nodes
- Expert view on Schmorl’s hernia therapy
- Methods for diagnosing Schmorl’s nodes
- Methods of treating Schmorl’s hernia
- Preventive measures for Schmorl’s node
- Amazing Aspects of Schmorl’s Nodes
- FAQ
Understanding Schmorl’s Hernia: Essence and Features
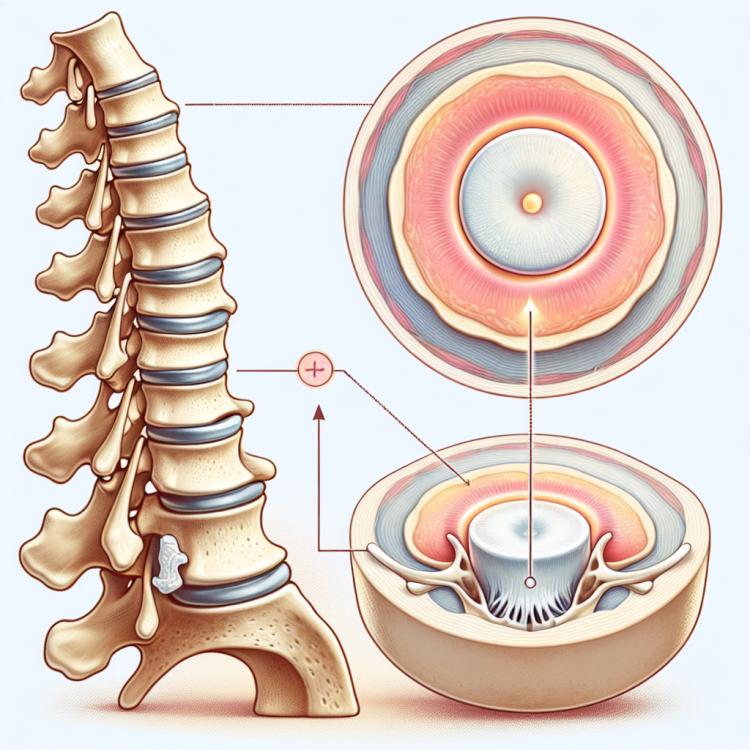
Schmorl’s hernia is a pathological condition in which there is a protrusion of the intervertebral disc through the body of the vertebra. The main sign of this process is the compression of the disc and its penetration into the bony tissue of the vertebra. This condition most commonly occurs in the thoracic spine and may be accompanied by painful sensations, sensory disturbances, and motor impairments in the area innervated by the affected nerve structures.
Understanding Schmorl’s hernia leads to the recognition of the importance of early diagnosis and a comprehensive approach to the treatment of this disease. Based on this, it is recommended to seek timely consultation with specialists and to apply appropriate correction and rehabilitation methods to prevent possible complications and restore the functions of the spinal column.
Etiology of Schmorl’s Hernia
Schmorl’s hernia is a form of spinal dorsopathy characterized by the protrusion of intervertebral disc nuclei into the vertebral body. This process usually occurs due to trauma or injuries that lead to damage to the structure of the cartilage rings of the discs, allowing the nucleus to extend beyond their limits.
The main causes of Schmorl’s hernia development include injuries, damage due to overstretching of the spine, genetic predisposition, and degenerative changes. Under the influence of these factors, discs can be squeezed into the vertebral bodies, causing not only pain and discomfort but also deformities of the spine.
- Injuries: Damage to the spinal column resulting from accidents, falls, or sports injuries can contribute to the development of Schmorl’s hernia.
- Overstrain injuries: Prolonged overload or insufficient unloading of the spinal column can lead to disc degeneration and, consequently, the possible extrusion of their nuclei.
- Genetic predisposition: Hereditary factors may also play a role in the development of Schmorl’s hernia, as some individuals may have weaker discs, increasing the likelihood of nucleus extrusion.
- Degenerative changes: With aging, the spinal discs are prone to wear and degenerative changes, which can contribute to the development of disc bulging and Schmorl’s hernia.
- Obesity: Excess weight creates additional pressure on the spine, which can increase the risk of developing Schmorl’s hernia by increasing the load on the discs.
The clinical picture of Schmorl’s nodes
Schmorl’s node often manifests without prominent clinical symptoms. However, some patients may experience symptoms such as back pain, urinary incontinence, numbness, or weakness in the limbs. Pain may worsen with physical activity or prolonged sitting or standing. The appearance of scoliosis or other spinal deformities is also possible.
The diagnosis of Schmorl’s node is based on the medical history, physical examination, and various instrumental methods, such as X-ray, magnetic resonance imaging, and computed tomography. Early detection and proper treatment of Schmorl’s node significantly affect the prognosis of the disease and help prevent potential complications.
- Back pain: patients often experience discomfort and pain in the back, which may worsen with physical activity.
- Urinary incontinence: some patients may encounter problems with bladder control due to pressure on the nerve structures in the lumbar region.
- Numbness and weakness in limbs: symptoms of numbness, weakness, or even loss of sensitivity in the legs or arms may occur due to compression of the nerve roots.
- Increased pain with prolonged sitting or standing: patients may notice increased pain in the lower back when sitting or standing in one position for a long time.
- Spinal deformities: irreversible changes in the structure of the spine, such as scoliosis or kyphosis, may manifest as a result of prolonged pressure from Schmorl’s hernia on the spinal column.
Expert view on Schmorl’s hernia therapy
Experts in the field of medicine tend to agree that the treatment of Schmorl’s hernia should be comprehensive and individualized depending on the clinical manifestations and characteristics of the patient. Sometimes, conservative treatment may be required to improve the patient’s condition, which includes physiotherapy, medications to reduce pain and inflammation, as well as recommendations for maintaining an activity regimen and proper posture.
However, in severe cases and in the presence of complications, surgical intervention may be necessary. Experts emphasize the importance of timely detection and adequate treatment of Schmorl’s hernia to prevent further complications and improve the quality of life for patients.

Methods for diagnosing Schmorl’s nodes
For the accurate diagnosis of Schmorl’s nodes, various examination methods are used, including spinal X-rays to detect deformities and changes; magnetic resonance imaging, which provides detailed images of the intervertebral discs and allows for the determination of the hernia’s spread; and computed tomography for more precise visualization of the area of damage. A clinical review of symptoms and physical examination also play an important role in the diagnosis of Schmorl’s nodes.
Correct diagnosis of Schmorl’s nodes is crucial for determining the treatment strategy and preventing complications. The combination of various diagnostic methods allows doctors to gain a comprehensive understanding of the condition of the intervertebral discs and to determine the optimal therapy plan for each individual case.
- X-ray of the spine: is conducted to identify deformities and changes in the structure of the spinal column.
- Magnetic resonance imaging (MRI): provides detailed images of intervertebral discs and helps determine the exact location and size of the hernia.
- Computed tomography (CT): allows for more detailed imaging of damaged tissues and structures of the spinal column.
- Clinical review of symptoms: the doctor analyzes the patient’s complaints, performs a physical examination, and assesses the nature of the pain and other manifestations.
- Assessment of the patient’s general condition: includes analyzing the medical history, studying the presence of hereditary diseases, and identifying possible risk factors.
Methods of treating Schmorl’s hernia
In cases where conservative methods do not bring improvements or if there are serious complications, surgical intervention may be required. Surgery for Schmorl’s hernia may involve the removal of damaged discs or stabilization of the spine. The decision on the treatment method is usually made by the doctor based on the clinical manifestations of each specific case and discussed with the patient.
- Conservative treatment: Includes rest, physical therapy, braces to support the spine, and anti-inflammatory medications.
- Physical therapy: Aims to strengthen back muscles to reduce pressure on intervertebral discs and alleviate symptoms.
- Injections: Used to reduce inflammation in the area of the hernia and decrease pain syndrome.
- Surgical intervention: May involve removing damaged discs or stabilizing the spine in cases where conservative methods are ineffective.
- Individual approach: The choice of treatment method is typically made by the physician taking into account clinical manifestations and is discussed with the patient to select the optimal therapy plan.
Preventive measures for Schmorl’s node
Controlling risk factors such as obesity and lack of physical activity is also an important component of preventing Schmorl’s Hernia. Regular consultations with a doctor to monitor the condition of the spine and timely treatment of other spinal diseases also contribute to hernia prevention and maintaining back health.
- Physical activity: Regular exercises to strengthen the back muscles and proper execution of physical loads contribute to maintaining spinal health.
- Proper posture: Maintaining proper posture while sitting, standing, and walking helps prevent stress on the spine and the discs between the vertebrae.
- Avoiding improper weight lifting: When lifting heavy objects, one should use the correct technique to avoid placing additional stress on the spine and discs.
- Weight control: Maintaining a healthy weight reduces pressure on the spine, which can decrease the risk of developing a hernia.
- Regular back examinations: Consultations with a doctor and monitoring the condition of the spine will help timely identify and prevent pathologies, contributing to back health maintenance.
Amazing Aspects of Schmorl’s Nodes
What’s also interesting is that Schmorl’s hernia often remains asymptomatic or presents with minimal manifestations, complicating diagnosis. However, modern examination and treatment methods provide opportunities for early detection and effective management of this condition, highlighting the importance of understanding this pathology for both specialists and patients.