Myocardial infarction: causes, symptoms, and treatment methods
- Definition and Causes of Myocardial Infarction
- Risk factors for the occurrence of myocardial infarction
- Main manifestations of myocardial infarction
- Expert opinion on the treatment of myocardial infarction
- Methods for diagnosing myocardial infarction
- Methods of treating myocardial infarction
- Measures for the prevention of myocardial infarction
- Unusual aspects of myocardial infarction
- FAQ
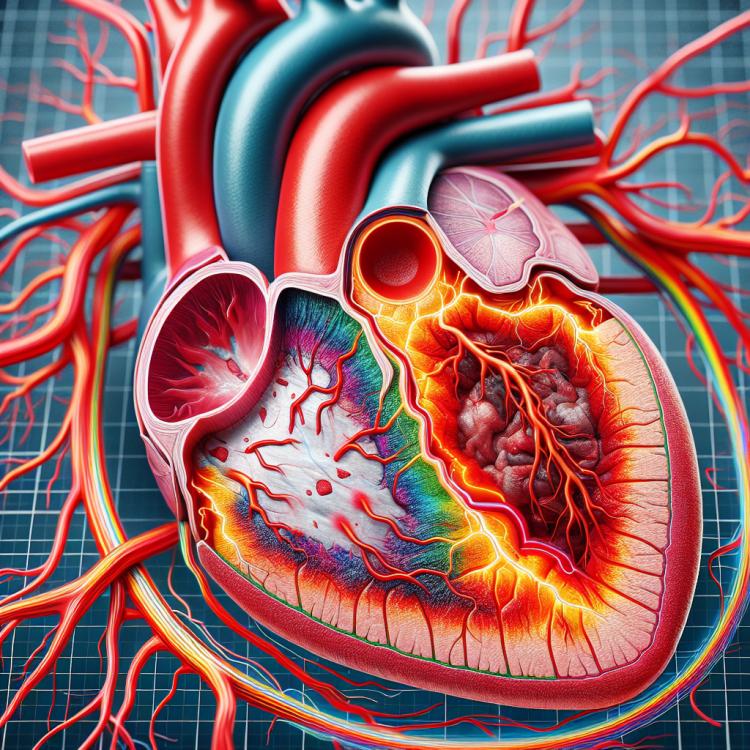
Definition and Causes of Myocardial Infarction
Myocardial infarction is an acute pathology of the cardiovascular system characterized by necrosis of the myocardial tissue due to impaired blood supply. The causes of its occurrence include obstruction of the coronary arteries due to thrombosis or embolism, which leads to a critical reduction in the supply of oxygen to the heart muscle and, consequently, to ischemia and necrosis of the myocardial tissue.
Other factors that contribute to the development of myocardial infarction may include atherosclerosis of the coronary arteries, arterial hypertension, uncontrolled diabetes, as well as elevated blood cholesterol levels. Understanding these mechanisms allows for a better description of the process of myocardial infarction and the development of effective strategies for the prevention of this disease.
Risk factors for the occurrence of myocardial infarction
The causes of myocardial infarction are usually associated with a combination of risk factors, including atherosclerosis, hypertension, diabetes, obesity, certain metabolic disorders, and some genetic factors. Atherosclerosis is the primary process leading to the formation of a thrombus that blocks blood flow in the coronary arteries, resulting in a myocardial infarction. Controlling risk factors, such as maintaining a healthy lifestyle, medication therapy, and dietary changes, plays an important role in the prevention of myocardial infarction.
- Atherosclerosis: Disorders of lipid metabolism contribute to the formation of atherosclerotic plaques in the arteries, increasing the risk of myocardial infarction.
- Hypertension: Elevated blood pressure puts additional strain on the heart, increasing the likelihood of myocardial infarction.
- Diabetes: High levels of glucose in the blood increase the risk of damage to blood vessels and heart muscle, contributing to the development of myocardial infarction.
- Obesity: Excess weight puts pressure on the heart, raising the risk of cardiovascular diseases, including myocardial infarction.
- Some genetic factors: Heredity may play a role in the predisposition to atherosclerosis and other risk factors for myocardial infarction.
Main manifestations of myocardial infarction
The main symptoms of a heart attack include chest pain, which may be described as pressure, squeezing, or burning pain, often radiating to the left shoulder, elbows, jaw, or back. Patients may also experience shortness of breath, loss of consciousness, nausea, and a feeling of unusual weakness. In some cases, the symptoms of a heart attack may be atypical, especially in elderly patients or individuals with diabetes, which can complicate the diagnosis of the condition and requires additional attention from medical staff.
- Chest pain: the symptom may be described as pressure, discomfort, squeezing, or burning in the chest area, radiating to the left arm, neck, jaw, or back.
- Shortness of breath: patients may experience difficulty breathing, a feeling of not having enough air during physical activity or at rest.
- Nausea and vomiting: symptoms accompanied by a feeling of nausea may occur during a myocardial infarction.
- Feeling of weakness and fatigue: patients may experience unexplained weakness, lethargy, or tiredness that may be related to a myocardial infarction.
- Loss of consciousness: in some cases of myocardial infarction, patients may lose consciousness due to impaired blood supply to the brain.
Expert opinion on the treatment of myocardial infarction
There is currently a broad consensus among leading medical specialists regarding the effectiveness and importance of early medical treatment of myocardial infarction, which includes aspirin, thrombolytics, beta-blockers, as well as angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor antagonists. Interventions aimed at restoring the patency of the blocked vessel (percutaneous coronary interventions or coronary bypass surgery) are also actively recommended for patients with myocardial infarction. However, the early diagnosis and immediate initiation of treatment tailored to the specific clinical case remain priorities in the treatment of myocardial infarction within the framework of modern medical practice.

Methods for diagnosing myocardial infarction
Various methods are used for the diagnosis of myocardial infarction, including electrocardiography (ECG), biomarkers of myocardial damage (such as troponins and creatine phosphokinase-MB), echocardiography, and coronary angiography. ECG is one of the main methods for confirming myocardial infarction, as it reflects changes in the electrical activity of the heart. Biomarkers of myocardial damage, such as troponins, are often used to assess the level of damage to the heart muscle. Echocardiography can evaluate the structure and function of the heart, including checking for the presence of thrombus formation. Coronary angiography is an invasive method that can directly visualize obstruction of the coronary arteries. The combination of these methods enables accurate and timely diagnosis of myocardial infarction and determines the optimal treatment for the patient.
- Electrocardiography (ECG): ECG records the electrical activity of the heart, revealing characteristic changes that may indicate a myocardial infarction.
- Cardiac injury biomarkers: Troponins, creatine phosphokinase-MB, and other biomarkers are used to assess damage to the heart muscle.
- Echocardiography: This is an educational diagnostic method that helps assess the structure and function of the heart, including the detection of blood clots and other anomalies.
- Coronary angiography: An invasive method for visualizing the coronary arteries, allowing for the determination of the extent and location of atherosclerotic plaques and obstructions.
- Television system monitoring: Special wearable devices can be used for continuous monitoring of heart activity and detection of changes indicating a myocardial infarction.
Methods of treating myocardial infarction
- Emergency methods for restoring myocardial blood supply: Include thrombolytic therapy and coronary angioplasty for the rapid restoration of blood flow to the heart muscle.
- Medication treatment: Includes the use of drugs to improve heart perfusion, reduce heart load, and prevent possible complications.
- Dietary recommendations: Are important for controlling cholesterol and blood pressure, reducing the risk of recurrent heart attack, and improving related conditions.
- Abandoning bad habits: Including smoking, as it reduces the risk of developing cardiovascular diseases and improves overall health.
- Physical exercises: Under medical supervision help strengthen the cardiovascular system, improve physical condition, and reduce the risk of heart dysfunctions.
Measures for the prevention of myocardial infarction
- Healthy lifestyle: regular physical exercise, healthy eating, and avoiding bad habits reduce the risk of myocardial infarction.
- Cholesterol level control: monitor your blood cholesterol levels, avoid fatty and high-calorie foods.
- Blood pressure monitoring: regular blood pressure checks help detect and manage hypertension in a timely manner, which reduces the risk of myocardial infarction.
- Quit smoking: smoking increases the risk of cardiovascular diseases, including myocardial infarction; quitting smoking positively affects heart health.
- Limit alcohol consumption: moderate alcohol consumption is recommended, but excessive intake may increase the risk of myocardial infarction; practice moderation when consuming alcohol.