Intussusception of the intestine: symptoms, diagnosis, and treatment methods
- Analysis of the concept: Intestinal intussusception
- Etiology of intestinal intussusception
- The clinical picture of intestinal intussusception
- Expert opinion on the treatment of intestinal invagination
- Methods for diagnosing intestinal invagination
- Methods of treating intestinal intussusception
- Prevention measures for intestinal invagination
- Amazing aspects of intestinal invagination
- FAQ
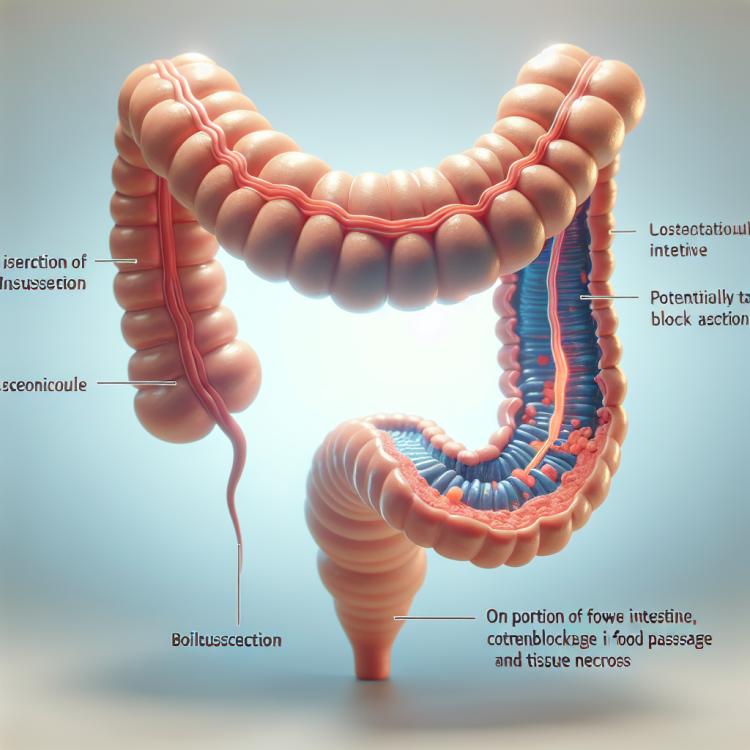
Analysis of the concept: Intestinal intussusception
Intestinal intussusception is a pathological condition in which a segment of the intestine turns inside out and pulls into the next segment, thus creating six layers of the intestinal wall. This can lead to circulatory impairment and tissue necrosis. Symptoms include acute abdominal pain, defecation disturbances, vomiting, and bleeding. Diagnosis is based on clinical manifestations and examination methods, including ultrasound. Treatment includes conservative methods aimed at eliminating the intussusception and, in severe cases, surgical intervention to restore normal intestinal anatomy and prevent complications.
Etiology of intestinal intussusception
Intestinal invagination, or telescoping of the intestine, is a serious condition characterized by the internal “folding” or insertion of a section of the intestine into an adjacent part of the intestine. The causes of invagination can be diverse, most frequently associated with intestinal pathologies such as polyps, tumors, inflammation, or hyperplasia of lymphoid tissue. Congenital anomalies or inflammatory processes can also contribute to the occurrence of intestinal invagination. The exacerbation of these factors can lead to invagination, necessitating surgical intervention to eliminate the dangerous condition.
- Polyps: The presence of polyps in the intestine may contribute to the occurrence of intussusception.
- Tumors: Malignant tumors or other neoplasms in the intestine may be a risk factor for the development of intussusception.
- Inflammatory processes: Chronic intestinal inflammations, such as ulcerative colitis or Crohn’s disease, may contribute to the development of intussusception.
- Congenital anomalies: Some congenital defects or anomalies of the intestine may increase the risk of intussusception.
- Lymphoid tissue hyperplasia: An increase in lymphoid tissue in the intestine may be associated with intussusception and its development.
The clinical picture of intestinal intussusception
Intestinal intussusception manifests a wide range of symptoms, including severe abdominal pain that can vary in nature from dull to sharp and colicky. Patients often complain of vomiting, heartburn, blood in the stool, as well as changes in peristalsis and bowel movements. Some patients may experience abdominal distension, elevated temperature, and shock in severe cases of intestinal intussusception.
Additionally, signs of intestinal obstruction may be observed with intussusception, such as the absence of gas and stool, development of intestinal paresis or peritonitis. Since the symptoms of intestinal intussusception can be diverse and serious, it is important to seek medical attention promptly for diagnosis and treatment of this condition.
- Intense abdominal pain: ranging from dull to sharp, with possible attacks.
- Vomiting: may be accompanied by heartburn and blood in the vomit.
- Changes in peristalsis: possible sections of the intestine with obstructions and ileus.
- Abdominal distension: patients often experience an increase in abdominal volume.
- Increased temperature and shock state: possible in severe cases of intestinal invagination.
Expert opinion on the treatment of intestinal invagination
Treatment of intestinal intussusception requires a comprehensive approach considering the clinical picture of each specific case. Experts note that when choosing a treatment method, the degree of intussusception development, the presence of complications, and the overall condition of the patient are taken into account. Surgical intervention is often urgent in cases where conservative methods do not yield the desired effect or if intestinal obstruction has already developed.
Experts also recommend timely diagnosis and treatment of the causes of intussusception, such as tumors, polyps, or inflammatory processes, to prevent recurrences. It is important to conduct postoperative monitoring and rehabilitation of the patient to prevent complications and ensure successful recovery after surgical intervention.

Methods for diagnosing intestinal invagination
The diagnosis of intestinal invagination includes various methods, starting with clinical examination and history. The specialist conducts a physical examination of the patient, identifying signs of abdominal tenderness, the presence of peristalsis, and other symptoms characteristic of invagination. Clinical diagnostic methods may be supplemented by laboratory studies, such as blood and urine tests, to assess the general condition of the patient and identify signs of inflammation or infection.
To accurately establish the diagnosis of intestinal invagination, the specialist may use instrumental methods, including ultrasound, computed tomography (CT), or X-ray. These methods allow for the visualization of the condition of the intestines, identify the presence of invagination, determine its extent, and choose the optimal treatment method for the patient.
- Clinical examination: The doctor conducts a physical examination of the patient, identifying signs of abdominal pain and other characteristic symptoms.
- Laboratory studies: Blood and urine tests can help assess the overall condition of the patient and detect signs of infection or inflammation.
- Ultrasound examination: Ultrasound can be used to visualize the intestines and identify intussusception.
- Computed tomography (CT): CT scanning helps to study the condition of the intestines in more detail and detect the presence of intussusception.
- X-ray: X-ray examination can be conducted to diagnose intestinal intussusception and determine its characteristics.
Methods of treating intestinal intussusception
An important aspect of treating intussusception is post-operative monitoring and rehabilitation of the patient. After surgical intervention, it is essential to strictly follow the physician’s recommendations, take medications, control nutrition, and monitor overall health. Patients are often prescribed rehabilitation activities, including physiotherapy, dietary therapy, and other recovery methods after surgery for intestinal intussusception removal.
- Surgical intervention: In cases where conservative methods are ineffective or in the presence of complications, surgery is performed to restore the correct position of the intestines and eliminate the causes of intussusception.
- Medication treatment: After surgery, patients may be prescribed medications to improve digestion, manage pain, antibiotics for infections, or other medications depending on their health status.
- Rehabilitation activities: After surgery, it is important to follow the doctor’s recommendations, maintain a proper diet, and undergo physiotherapy to speed up recovery after the procedure.
- Diet therapy: Specialists may prescribe a special diet aimed at easing the workload on the digestive system and aiding recovery after surgery to correct intestinal intussusception.
- Follow-up observation and regular consultations: After successful treatment, the patient should undergo follow-up observation with the doctor to assess the effectiveness of the treatment, prevent recurrences, and maintain overall health.
Prevention measures for intestinal invagination
In addition, regular physical exercise and maintaining a healthy lifestyle also play an important role in the prevention of intestinal intussusception. Strengthening the abdominal muscles and maintaining overall bowel tone help prevent the possibility of the bowel folding and improve its functioning. Following the doctor’s recommendations, properly treating chronic gastrointestinal diseases, as well as regular medical check-ups, can also help reduce the risk of intestinal intussusception.
- Balanced nutrition: Consuming foods rich in dietary fiber promotes normal bowel function and reduces the risk of developing conditions that contribute to intussusception.
- Drinking enough water: Regular fluid intake helps maintain normal digestion and prevents constipation, which can be a risk factor for intussusception.
- Physical activity: Regular exercises aimed at strengthening the abdominal muscles and overall tone of the digestive organs contribute to improved peristalsis and the prevention of intussusception.
- Maintaining a healthy lifestyle: Avoiding harmful habits, monitoring weight and overall physical condition helps prevent a range of gastrointestinal diseases, including intestinal intussusception.
- Regular medical check-ups: Visiting a doctor for preventive examinations, monitoring chronic diseases, timely screenings, and consultations help identify problems at an early stage and prevent possible complications, including intestinal intussusception.
Amazing aspects of intestinal invagination
Another interesting fact is that surgical intervention for intestinal invagination is often urgent, especially in cases of complications or signs of bowel obstruction. Performing the surgery requires a high level of qualification from surgeons, an accurate diagnosis, and timely actions to prevent complications and preserve the patient’s health. These aspects of intestinal invagination highlight the need for a deep understanding and prompt resolution of the issue when this condition arises.