Ischemic heart disease (IHD) – causes, symptoms, and modern treatment methods
- Explanation of Ischemic Heart Disease (IHD)
- Factors contributing to the development of CAD
- The main symptoms of Ischemic heart disease (IHD)
- Expert opinion on the treatment of Ischemic Heart Disease (IHD)
- Methods for diagnosing Ischemic Heart Disease (IHD)
- Effective treatment of Ischemic Heart Disease (IHD)
- Prevention measures for Ischemic Heart Disease (IHD)
- Funny facts about Ischemic Heart Disease (IHD)
- FAQ
Explanation of Ischemic Heart Disease (IHD)
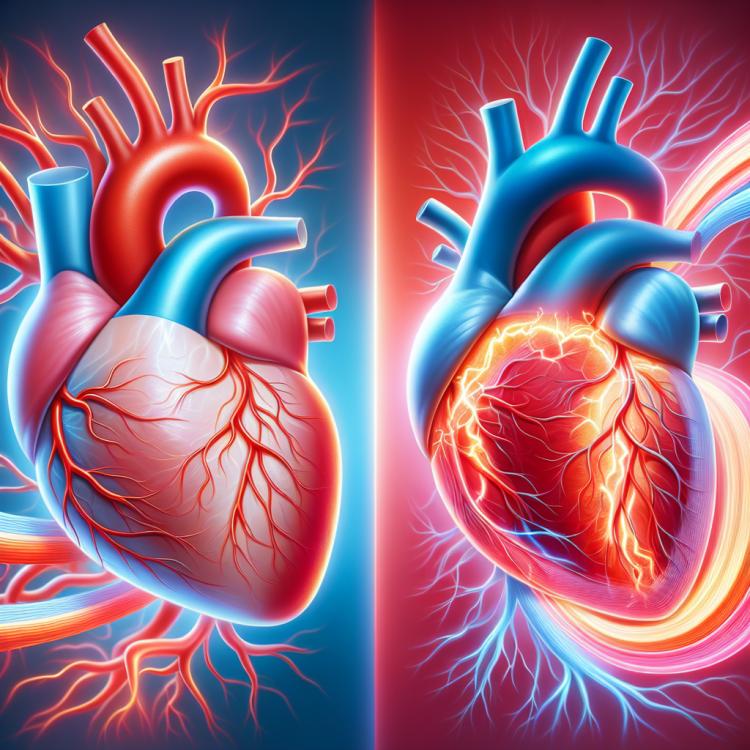
Ischemic heart disease (IHD) is a condition characterized by impaired blood supply to the heart muscle due to narrowing or blockage of the coronary arteries. This results in insufficient oxygen and nutrients needed for the normal functioning of the heart. The main causes of IHD are atherosclerosis and thrombus formation, which can obstruct or completely halt blood flow in the heart’s arteries, leading to ischemia and ischemic attacks.
IHD often manifests during physical activity or stress, accompanied by symptoms such as burning chest pain (angina), shortness of breath, and fatigue. Diagnosis of IHD includes ECG, exercise tests, and coronary angiography. Treatment may include medication therapy, surgical interventions (such as bypass surgery, angioplasty), or rehabilitation measures to improve the overall condition of the patient and prevent complications.
Factors contributing to the development of CAD
Ischemic heart disease (IHD) is a serious condition caused by impaired blood supply to the heart muscle due to stenosis (narrowing) of the coronary arteries. The main factors contributing to the development of IHD are atherosclerosis (the deposition of fatty plaques on the walls of blood vessels), hypertension (increased blood pressure), diabetes, cholesterol levels, tobacco smoking, obesity, insufficient physical activity, and stressful conditions. The combination of these factors can lead to reduced blood supply to the heart, the development of atherosclerosis in the coronary arteries, and ultimately to the development of IHD.
- Atherosclerosis: the deposition of fatty plaques on the walls of arteries leads to a narrowing of the vessel lumen and disruption of blood flow to the heart.
- Hypertension: high blood pressure increases the workload on the heart and may contribute to the development of coronary artery disease.
- Diabetes: diabetes is a significant risk factor for cardiovascular diseases, including coronary artery disease.
- Cholesterol level: high levels of “bad” cholesterol (LDL) may contribute to the formation of atherosclerotic plaques in the arteries.
- Smoking: nicotine and other toxic substances in tobacco smoke increase the risk of developing atherosclerosis and coronary artery disease.
The main symptoms of Ischemic heart disease (IHD)
The main symptoms of Ischemic Heart Disease (IHD) may include angina, or a feeling of pressure, squeezing, or pain in the chest that may radiate to the neck, arm, back, or abdomen. Patients may also experience feelings of shortness of breath, fatigue, weakness, as well as unusual heartbeats. Some patients may find it uncomfortable to feel pulsation in the neck or abdomen. Depressed mood, stress, and anxiety may also accompany IHD symptoms.
It is important to note that in some patients, particularly in women and the elderly, IHD symptoms may manifest less obviously or may include unusual manifestations such as nausea, vomiting, unusual weakness, or fatigue. Changes in typical IHD symptoms may also be an indicator of a more serious condition requiring immediate medical attention.
- Angina: a symptom of brief acute pain that may radiate to the neck, arms, back, or abdomen.
- Shortness of breath: occurring during physical exertion or at rest, may be a consequence of insufficient blood supply to the heart.
- Fatigue and weakness: a feeling of general tiredness and weakness without obvious reasons, possibly due to inadequate oxygen in the body.
- Palpitations: the sensation of unusual heartbeats or abnormal heart rate.
- Pulsation: an unpleasant feeling of pulsation usually in the neck or abdomen, may be associated with circulation disorders.
Expert opinion on the treatment of Ischemic Heart Disease (IHD)
Expert opinion on the treatment of Ischemic Heart Disease (IHD) emphasizes the importance of a comprehensive approach to managing this condition. Experts recommend combining pharmaceutical therapy, lifestyle changes, and sometimes surgical intervention to effectively control symptoms and reduce the risk of complications. This includes the use of medications to lower blood pressure, cholesterol levels, and control blood coagulation, as well as recommendations for healthy eating, physical activity, and weight management.
Experts also highlight the necessity of regular monitoring of patients with IHD to respond promptly to changes and adjust treatment accordingly. In the presence of severe symptoms or ongoing disease progression, experts advise consulting qualified cardiologists for assessment and making optimal treatment decisions for IHD.

Methods for diagnosing Ischemic Heart Disease (IHD)
To diagnose Ischemic Heart Disease (IHD), experts can use various methods, including electrocardiography (ECG), stress tests, coronary angiography, and routine blood cholesterol level tests. ECG allows for the assessment of the heart’s electrical activity, while stress tests help determine the heart’s response to physical activity. Coronary angiography provides the opportunity for a visual representation of the condition of the coronary arteries and identifying narrowed areas, while cholesterol measurements help assess the risk of atherosclerosis and its connection to IHD.
Additional methods, such as echocardiography (heart ultrasound), magnetic resonance imaging (MRI) of the heart, and angiography, may also be employed for more detailed diagnosis and characterization of myocardial damage in IHD. These methods provide a more comprehensive view of the patient’s heart condition and assist in choosing optimal treatment methods and recommendations for disease management.
- Electrocardiography (ECG): ECG is used to record the electrical activity of the heart and can show signs of ischemia.
- Stress tests: These tests are conducted to assess the heart’s response to physical activity and can help detect hidden coronary heart disease (CHD).
- Coronary angiography: This procedure allows for a visual assessment of the condition of the coronary arteries and to detect areas of stenosis or occlusion.
- Blood cholesterol level measurements: Monitoring cholesterol levels can help assess the risk of atherosclerosis and its relationship to the development of CHD.
- Transthoracic echocardiography (heart ultrasound) and Magnetic Resonance Imaging (MRI): These methods provide more detailed information about the structure and function of the heart and can also detect changes associated with CHD.
Effective treatment of Ischemic Heart Disease (IHD)
Interventional procedures, such as coronary artery bypass surgery and angioplasty, are aimed at restoring normal blood flow to the heart and reducing angina. Coronary artery bypass surgery involves creating a detour around narrowed sections of the arteries using a graft from the patient’s own vessels or using artificial grafts. Angioplasty helps to widen narrowed sections of the arteries using a small balloon or stents. A combination of drug therapy, procedures, and lifestyle changes can be key to the successful management of IHD and improving the prognosis for patients.
- Medications: Include aspirin for blood thinning, cholesterol-lowering medications, beta-blockers for controlling arrhythmia and improving heart function, as well as medications for lowering blood pressure.
- Coronary bypass surgery: A procedure aimed at creating a detour around narrowed arteries, providing better blood supply to the heart.
- Angioplasty: A method of widening narrowed sections of arteries using a balloon or stents to improve blood flow to the heart.
- Revascularization procedures: Include percutaneous coronary intervention (PCI) to widen stenoses and restore blood flow in the heart arteries.
- Lifestyle changes: Weight control, healthy eating, physical activity, quitting smoking, and regular medical check-ups are essential components of effective treatment for coronary heart disease.
Prevention measures for Ischemic Heart Disease (IHD)
Regular medical check-ups, especially for individuals at higher risk of developing IHD (e.g., patients with diabetes or hypertension), allow for the identification of risk factors and the initiation of timely treatment to prevent the possible development of the disease. Preventing obesity, managing stress, effectively managing chronic diseases, and promptly consulting a doctor when unusual symptoms arise also contribute to the prevention of IHD and improve the overall condition of the cardiovascular system.
- Healthy lifestyle: leading an active lifestyle, balanced nutrition, giving up harmful habits such as smoking, and moderate alcohol consumption help reduce the risk of developing coronary heart disease.
- Regular physical activity: physical activity improves the cardiovascular system, lowers cholesterol and blood pressure levels, which is important for the prevention of coronary heart disease.
- Monitoring cholesterol and blood pressure levels: regular medical check-ups allow for the detection and monitoring of cholesterol and blood pressure levels, reducing the risk of cardiovascular diseases, including coronary heart disease.
- Preventing obesity: maintaining a healthy weight and reducing excess fat deposits help lessen the load on the heart and blood vessels.
- Stress management: stress can negatively affect the cardiovascular system, so it’s important to find ways to cope with stress and maintain psychological and emotional balance.
Funny facts about Ischemic Heart Disease (IHD)
Another interesting fact is that risk factors for IHD, such as hypertension, diabetes, and high cholesterol, are increasingly observed among young people, highlighting the importance of focusing on the prevention of cardiovascular diseases from a young age. Understanding the characteristics of the development and progression of IHD will aid in the fight against this disease and help prevent its occurrence.