Esophageal ulcer: causes, symptoms, and treatment methods
- Understanding Esophageal Ulcers: Key Aspects and Symptoms
- Etiology of esophageal ulcer
- The main signs of esophageal ulcer
- Expert opinion on methods of treating esophageal ulcer
- Methods of diagnosing esophageal ulcer
- Methods for treating esophageal ulcer
- Prevention measures for esophageal ulcers
- Amazing aspects of esophageal ulcers
- FAQ
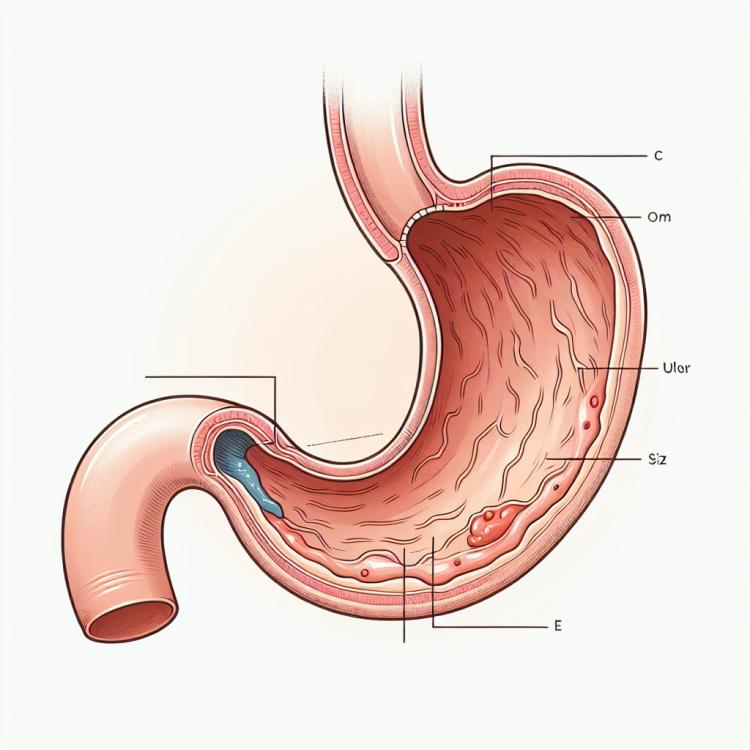
Understanding Esophageal Ulcers: Key Aspects and Symptoms
Esophageal ulcer is an ulcerative lesion of the mucous membrane of the esophagus, predominantly caused by the action of gastric juice or gastroesophageal reflux. This pathological process may be accompanied by symptoms such as heartburn, pain when swallowing, and a feeling of fullness or heaviness in the epigastric area. Despite its similarity to the symptoms of gastric ulcer, esophageal ulcer has its own characteristic manifestations and therefore requires an individualized diagnostic and therapeutic approach.
Understanding esophageal ulcer involves identifying the main causes of the disease, precise diagnosis using endoscopic methods, and determining a treatment strategy aimed at alleviating symptoms, healing the ulcer defect, and preventing recurrences. In the context of clinical practice, a critical understanding of the main aspects of esophageal ulcer not only allows for optimal management of this disease but also reduces the risk of complications and increases the effectiveness of treatment.
Etiology of esophageal ulcer
Esophageal ulcer is a serious condition that is often caused by an imbalance between aggressive and protective factors of the esophageal mucosa. Among the main causes of esophageal ulcer are Helicobacter pylori infection, prolonged use of certain medications (such as NSAIDs), smoking, alcohol consumption, stressful situations, and gastroesophageal reflux. Additionally, genetic predisposition and immune system disorders may also contribute to the development of esophageal ulcer.
Understanding the etiology of esophageal ulcer is important for the proper approach to the treatment and prevention of this condition. Identifying the main causes that contribute to the development of the ulcer allows for effective correction of risk factors and taking necessary measures to prevent complications from arising. Therefore, it is important to strive for a complete understanding of the mechanisms underlying the etiology of esophageal ulcer to ensure the most effective and targeted treatment of this disease.
- Helicobacter pylori infection: the presence of this bacterium in the stomach is associated with the development of esophageal ulcers.
- Long-term use of NSAIDs: non-steroidal anti-inflammatory drugs can negatively affect the esophageal mucosa, contributing to the formation of ulcers.
- Smoking: tobacco smoke can damage the esophageal lining, increasing the likelihood of ulcer development.
- Alcohol consumption: excessive alcohol consumption can exacerbate inflammatory processes in the esophagus, raising the risk of ulcer formation.
- Gastroesophageal reflux: the backflow of stomach contents into the esophagus can cause irritation and damage to its walls, contributing to the formation of ulcers.
The main signs of esophageal ulcer
The symptoms of esophageal ulcer can vary depending on the degree and location of mucosal damage in the esophagus. One of the main signs is a burning sensation or pain in the chest area, which usually intensifies after eating. Patients with esophageal ulcer may also experience dysphagia (difficulty swallowing), heartburn, and a feeling of heaviness in the epigastric region. Additionally, some patients may experience vomiting, nausea, anemia, or weight loss, which can also indicate the presence of an esophageal ulcer.
The diagnosis of esophageal ulcer includes performing esophagogastroduodenoscopy (EGD) to visualize mucosal damage. Furthermore, patients may undergo additional tests, such as tests for Helicobacter pylori infection and blood tests to determine hemoglobin levels and the presence of antibodies. Given the variety of symptoms associated with esophageal ulcer, it is important to seek medical help in a timely manner for a comprehensive examination and appropriate treatment.
- Chest pain: patients with esophageal ulcers may experience a burning sensation or pain in the chest, especially after eating.
- Dysphagia: difficulty swallowing may be one of the manifestations of an esophageal ulcer due to impaired passage through the esophagus.
- Heartburn: a feeling of hot or sour taste in the chest that occurs after eating may indicate an esophageal ulcer.
- Nausea and vomiting: some patients may experience nausea and vomiting, especially after eating, which may be related to an esophageal ulcer.
- Anemia and weight loss: an esophageal ulcer can lead to anemia due to blood loss or nutrient deficiencies, which may be accompanied by weight loss.
Expert opinion on methods of treating esophageal ulcer
Experts in the field of gastroenterology emphasize the importance of a comprehensive approach to the treatment of esophageal ulcers. Depending on the characteristics of the disease, doctors may recommend a combination of medication therapy, diet, risk factor management, and, in some cases, surgical intervention. An important part of treating esophageal ulcers is the eradication of Helicobacter pylori, as infection with this bacterium is often one of the primary causes of esophageal ulceration.
Experts also highlight the need for regular medical monitoring of patients after treatment is completed, to prevent recurrences and to timely detect complications. Special attention is given to managing risk factors such as alcohol consumption, smoking, stress, and the use of medications that contribute to the development of esophageal ulcers. Experts’ opinions are aimed at effective and safe treatment of esophageal ulcers with the goal of achieving long-term remission and improving the quality of life for patients.

Methods of diagnosing esophageal ulcer
For the diagnosis of esophageal ulcers, various methods are used, one of the main ones being esophagogastroduodenoscopy (EGDS). This procedural method allows visualization of the condition of the mucous membrane of the esophagus, stomach, and duodenum, which can be key in identifying ulcers and other pathologies of the digestive system. Other methods for diagnosing esophageal ulcers may include computed tomography (CT), contrast radiography, as well as tests for the presence of Helicobacter pylori through blood, urine, or mucosal tissue analyses.
It is important to note that accurate and timely diagnosis of esophageal ulcers plays a crucial role in prescribing effective treatment and preventing possible complications. Considering the variety of diagnostic methods, doctors select the optimal combination of studies, taking into account the individual characteristics of the patient, the degree of disease progression, and other factors for the most complete and precise identification of esophageal ulcers.
- Esophagogastroduodenoscopy (EGD): a method of visualizing the esophagus, stomach, and duodenum, allowing for the detection of ulcers and other pathologies.
- Computer Tomography (CT): a conducted study to assess the condition of the digestive system and identify possible ulcers.
- X-ray with contrast agent: a method that uses X-ray radiation to diagnose esophageal ulcers using a contrast medium.
- Tests for Helicobacter pylori infection: blood, urine, or tissue analyses to determine the presence of the bacteria associated with the development of esophageal ulcers.
- Barium X-ray: a diagnostic method in which the patient is given a contrast agent to drink for visualization of the gallbladder and the lumen of the esophagus.
Methods for treating esophageal ulcer
In addition to the treatment of Helicobacter pylori, patients with esophageal ulcers may be recommended the use of prokinetics to improve esophageal motility, as well as anti-inflammatory drugs and antacids to relieve symptoms. In some cases, where there are complications or ineffectiveness of conservative therapy, surgical intervention may be required. Targeted and timely treatment of esophageal ulcers under the supervision of specialists will help prevent complications and achieve long-term remission of the disease.
- Eradication therapy for Helicobacter pylori: Combined use of antibiotics and acid-suppressing medications to eliminate the H. pylori bacteria.
- Proton pump inhibitors and anti-secretory medications: Medications that reduce acid production in the stomach, helping to heal esophageal ulcers.
- Prokinetics: Drugs that stimulate stomach and esophageal motility to improve digestion.
- Anti-inflammatory medications and antacids: Used to relieve symptoms of esophageal ulcers, such as pain, heartburn, and dyspepsia.
- Surgical treatment: In cases of complications or ineffectiveness of conservative therapy, surgical intervention may be necessary to resect the ulcer or reconstruct the esophagus.
Prevention measures for esophageal ulcers
Regular screening tests to detect Helicobacter pylori infection, regulating the duration of medication use, as well as the application of gastroprotective agents in high-risk groups can be effective preventive measures against esophageal ulcers. It is important to consult a doctor to develop an individual prevention strategy based on the patient’s characteristics and medical history.
- Avoid smoking and alcohol consumption: Tobacco and alcohol can contribute to the development of esophageal ulcers, so their consumption should be minimized or completely excluded.
- Maintain a healthy diet: A proper diet rich in fruits, vegetables, and whole grains will help support the health of the digestive system and reduce the likelihood of developing ulcers.
- Avoid excessive stress: Stress can negatively impact the digestive system, so it is important to learn to manage stressful situations and apply relaxation methods to maintain emotional health.
- Regular screening examinations: Conducting tests for Helicobacter pylori infection and other risk factors allows for early detection of the disease and timely initiation of treatment.
- Follow doctor’s recommendations: It is important to consult with a doctor to develop an individual prevention program and regularly undergo examinations to monitor the condition of the esophagus and timely identify potential problems.
Amazing aspects of esophageal ulcers
There is also an interesting dynamic regarding the incidence of esophageal ulcerations related to lifestyle changes and the spread of information about risk factors. Increased attention to healthy eating, regular physical activity, as well as education about the dangers of smoking and excessive alcohol consumption contributes to a reduction in the number of esophageal ulcer cases in certain population groups.